I’ve wanted to help people with their health as far back as I can remember. I grew up watching my mom work as a medical doctor and always admired her. In elementary school, I was introduced to the scientific method and thought: “This is it! This is what I’m going to do when I grow up!”
I began to read about innovative health research as early as junior high, and hoped that I could one day dedicate my life’s work to science! I majored in science in undergrad, missing the Thursday night parties because I had to study for chemistry, biology, and physics pop quizzes that I had on most Friday mornings. But I didn’t mind! I was excited that I got to synthesize chemicals, grow cells in Petri dishes, and make electronic gadgets.
I then enrolled in a 4-year PharmD program (Doctor of Pharmacy) and became a pharmacist with the goal that one day I would be able to discover new treatments for people who were suffering. Not long after my graduation from pharmacy school, I was able to find a position that allowed me to grow my research skills and utilize my passion for helping people.
I worked as a consultant pharmacist at a case management center that helped people with disabilities and rare conditions. I loved to spend hours reading about various, often unknown, health conditions and treatments… and enjoyed solving pharmacological problems based on the person’s unique physiology.
Once I was diagnosed with Hashimoto’s, I turned my research skills and passion to getting myself — and, eventually, others with the condition — well. Instead of just masking my symptoms, I rebelled against the traditional Hashimoto’s “authorities” and set out to find the root cause of my condition.
Over the last several years, I’ve spent countless hours reading and analyzing every piece of research about Hashimoto’s that I could get my hands on.
I have to say… I love it! I felt like a kid coming out of a candy store when I received 680+ new research articles on Hashimoto’s and autoimmunity one day. You should have seen the grin on my face! I’ve learned so much from the published scientific studies.
But in addition to strictly scientific articles, I’ve also found a tremendous amount of value from simply listening to people with Hashimoto’s. I’ve learned so much from my clients and readers.
One important thing that I came to learn from my client work is that different people may have different root causes, but that there are also certain interventions that help most of us.
This thought process of looking at the interventions that help most is based on my work in public health, where I was trained in outcomes research. In very simple terms, outcomes research focuses on identifying a group of patients with a specific condition and tracking their health outcomes when certain clinical interventions were undertaken.
While clinical trials are excellent at tracking specific outcomes in relation to one intervention in a controlled setting (such as what happens to thyroid antibodies when the Blastocystis hominis infection is treated), outcomes research can track multiple interventions in a real world setting (i.e. What happens to a person’s symptoms, TSH, and antibodies when they start a gluten-free diet, selenium and adrenal adaptogens?).
I started tracking outcomes with my own clients back in 2013, to see which interventions were helpful (or harmful), and was excited when I collected around 100 surveys from my clients, that showed that lifestyle interventions were indeed helpful. I was planning on writing about this.
But then it occurred to me…
We, the empowered Hashimoto’s community of Root Cause Rebels, can create our own outcomes research! So in 2015, I conducted a survey of 2,232 people with Hashimoto’s and gathered the results to learn all that I could about what was working and not working for people. I have since used that information, along with my research, training in functional medicine, nerding out with other clinicians, and of course years of insights gathered from my clients, to help shape many of the recommendations that I share with my readers.
We’ve all had a little more time at home than usual lately, and if you’ve felt a little stuck in a rut with your health goals, now might be a great time to incorporate one or more interventions that are easy to “DIY” from the comfort of home. 🙂
Read on to learn about:
- How my Hashimoto’s diagnosis turned into my mission to heal
- Top 10 DIY interventions to feel better — from readers like you
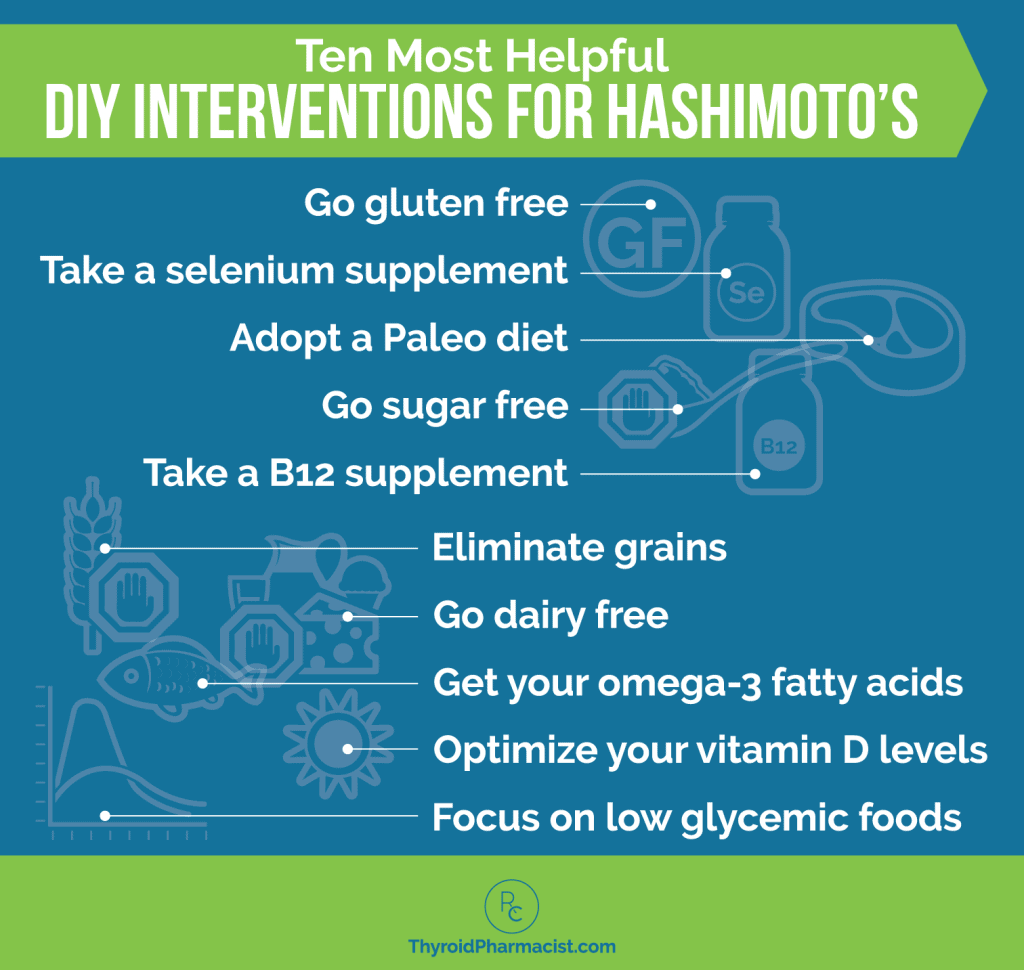
10 DIY Interventions for Hashimoto’s
There are so many different things that may or may not help a person with Hashimoto’s, that I think people can often get overwhelmed. Some of the interventions rely heavily on finding “Dr. Right”, but others can be done in the comfort of our own homes.
Here are the top ten DIY recommendations that came back from my survey. They are all easy to implement on your own, without a doctor’s prescription (though you may want to look into ordering labs if you haven’t already), and can be some of the most effective tools for getting your own body into remission!
While there’s always a chance that a change in our lifestyle may lead to a worsening of symptoms, these interventions are very safe for most people who try them out in the real world.
People often ask me about why I don’t recommend high dose iodine supplements or the vegan diet on my website or in my books, and my answer is that there are almost as many people harmed as helped by these interventions. Thus, a person should not try them without knowledgeable supervision and lab testing. Meanwhile, the interventions below generally have a success rate of >60 percent and a harm rate of <1 percent.
1. Go Gluten Free
Food sensitivities can be a root cause for Hashimoto’s, and can result from a leaky gut that is always present with autoimmunity. Removing these reactive foods will often alleviate many of the symptoms associated with Hashimoto’s.
Gluten is one of the most common food sensitivities. Of the readers that responded to my survey, 88 percent of them felt better on a gluten-free diet!
After finding out that I had IgG (Immunoglobulin G antibodies) reactions to gluten (a protein found in wheat, rye and barley), as well as to the dairy proteins whey and casein, I came across a condition known as non-celiac gluten sensitivity (NCGS). With this type of sensitivity, people have celiac-like reactions to gluten, yet they don’t test positive to the typical IgA celiac antibodies, nor do they present the characteristic damage to intestinal cells seen in celiac disease.
Most of the readers that I surveyed said their gluten reactions had included gut issues like constipation, diarrhea, cramping, bloating, gas, nausea, and burning or burping from acid reflux, as well as brain-related symptoms such as headaches, brain fog, anxiety, depression, fatigue, and insomnia.
However, research has shown that there are many correlations between those with thyroid disease and gluten sensitivities. For example, a 2002 study in the European Journal of Endocrinology found that 43 percent of people with Hashimoto’s showed activated mucosal T cell immunity, which is usually correlated with gluten sensitivity.
There could be numerous reasons why a person may react to wheat products. Some of them include small intestinal bacterial overgrowth (SIBO), which results in an impaired ability to break down various food particles, including fructans. In fact, a recent study found that fructan, a food molecule that may be found in wheat, is to blame for NCGS symptoms, and not gluten.
Histamine intolerance, nickel sensitivity, and gut dysbiosis have all been tied to NCGS.
Another important point to make about gluten and autoimmune disease is that studies have shown that gluten induces intestinal permeability in all individuals, regardless of whether or not they have celiac disease. And we know that intestinal permeability (leaky gut) is a factor for everyone with Hashimoto’s. As such, removing gluten from one’s diet can be an easy yet highly effective DIY intervention to help you heal.
Thirty-three percent of respondents to my survey had a reduction in their thyroid antibodies on a gluten-free diet. Along with feeling better and seeing a reduction in antibodies, the biggest benefits seen in people with Hashimoto’s on the gluten-free diet were more energy (in 67 percent of people), a better mood (in 60 percent of people), and a healthier weight (in 52 percent of people).
As a pharmacist, I was surprised to see that more people reported improvements with the gluten-free diets in these domains, than they did with using thyroid replacement hormones!
Less than one percent of respondents reported feeling worse after going on a gluten-free diet, and 11 percent reported no noticeable changes.
To learn more about gluten and Hashimoto’s and why I recommend everyone with Hashimoto’s eliminate gluten from their diet, please see my gluten article.
Please note that eliminating gluten from your diet may cause a decrease in selenium intake… keep reading! 🙂
2. Take a Selenium Supplement
Selenium is an important trace element and antioxidant required for healthy thyroid hormone synthesis and metabolism. The human thyroid gland has been found to have the highest content of selenium per gram of tissue among all the organs in the human body. Selenium supports the conversion of your body’s inactive thyroid hormone thyroxine (T4) into the form your body needs, the biologically active triiodothyronine (T3). It protects your body’s thyroid cells from oxidative damage during this process.
Our bodies do get selenium from the foods we eat. According to one study, the main sources of selenium are meat products (31 percent), fish (19 percent), pasta or rice (12 percent), and bread or cereals (11 percent).
However, many people with Hashimoto’s may turn to a gut-friendlier diet such as a gluten-free or grain-free diet, lowering their selenium intake.
Reduced selenium levels have also been associated with the consumption of eggs, white rice, alcohol, and coffee, in addition to smoking.
Selenium deficiency is one of the most common nutrient deficiencies that I see in people with Hashimoto’s — research shows that most people with Hashimoto’s will have a deficiency in this key thyroid nutrient, and it is a very common and widely recognized trigger of autoimmune thyroid conditions.
This is likely because selenium absorption is affected by many of the same triggers and conditions commonly seen in Hashimoto’s (poor nutrient absorption, stress, toxins, gut infections, to name a few).
While the gluten-free diet has been found to improve Hashimoto’s symptoms and reduce the autoimmune attack on the thyroid as mentioned above, selenium deficiency can be caused or worsened by gluten and grain-free diets, as demonstrated in nutritional studies involving people with celiac disease, due to a decreased intake of grains and cereals.
The good news is that supplementing with selenium at a therapeutic dosage, has been found to reduce thyroid antibodies, reduce thyroid symptoms, and improve overall well-being.
When I surveyed my readers, 63 percent of respondents said that taking a selenium supplement helped them feel better.
Of those who saw improvement in their symptoms, 58 noticed more energy, 48 percent experienced better mood, 37 percent improved their labs, and 25 percent saw positive results in their body weight.
Another 4 percent reported that selenium made them feel worse, while 34 percent saw no changes.
Research suggests that selenium supplementation for people with Hashimoto’s is associated with a reduction in TPO antibody levels, improved thyroid ultrasound features, and improved quality of life.
In one study, 71 patients with Hashimoto’s (who also had high levels of antibodies), were treated. Half of the participants were given selenium supplementation at a dosage of 200 mcg per day, along with levothyroxine, for a 90 day period. The other half was only given levothyroxine and a placebo. The results showed that those with selenium supplementation showed a 40 percent decrease in TPO antibodies. The other group (placebo group) only showed a 10 percent decrease. In 24 percent of those taking a selenium supplement, antibody levels completely normalized! Those taking supplementation also reported better well-being compared to the placebo group.
Along with seeing a reduction in thyroid antibodies, I have found that selenium supplementation also often results in a reduction in anxiety in many people with Hashimoto’s.
Anxiety, irritability, and moodiness are all symptoms which are frequently associated with Hashimoto’s and Graves’ disease. I suffered from significant anxiety myself, but taking selenium supplements and balancing my blood sugar worked wonders at providing me a renewed sense of calm.
So, if this resonates with you, consider boosting your selenium levels with a supplement. It’s a “DIY” intervention that you can easily implement! I generally recommend Selenium Methionine from Pure Encapsulations at a dose of 200 mcg per day. It will typically take three to five days for symptoms to show improvement, and three full months to see a possible reduction in thyroid antibodies.
Because of the absorption issues many people have with their gut, I do always recommend people take a selenium supplement with a vitamin E supplement as well.
For more information about selenium and supplement precautions, please read my full article.
3. Go Dairy Free
When I surveyed my readers with Hashimoto’s, 40 percent of people reported already being dairy free, while 57 percent reported that they suspected they were sensitive to dairy.
The most common ways a dairy sensitivity may manifest are via gut reactions (like bloating, diarrhea, and acid reflux), as well as lung reactions (coughing, asthma, sinusitis, postnasal drip, and mucus) and skin reactions (eczema, rashes, and acne).
Cow’s milk contains proteins (primarily casein and whey) that are different from the proteins found in human milk. A person with intestinal permeability (which is always a precursor to autoimmune disease) is likely to recognize these proteins as a foreign invader and make IgG antibodies to the proteins to protect itself.
Some people with Hashimoto’s may present with an IgA (celiac-like) intolerance to milk proteins. Many of these cases are undiagnosed, and when people continue to eat these foods, they are damaging their intestines and robbing themselves of vital nutrients.
Many people with Hashimoto’s could have both kinds of immune reactions (IgG and IgA) to dairy proteins, in addition to an intolerance of lactose.
Dairy intolerance and lactose intolerance are often confused, and many people will suggest taking a Lactaid pill so that you can eat your ice cream and go about your day.
However, lactose intolerance and dairy protein intolerance are two completely different reactions to dairy. Lactose is a milk sugar, and the ability to digest lactose depends on having the lactase enzyme necessary to break down the milk sugar lactose.
Although there are similarities in the symptoms caused by lactose intolerance and dairy protein sensitivity (bloating, diarrhea), the difference is that the latter response originates in the immune system. Additionally, lactose intolerance will not cause intestinal tissue inflammation or damage.
Interestingly, a recent study showed that 76 percent of people with Hashimoto’s who were tested for lactose intolerance, tested positive. When they were placed on a lactose-free diet, their TSH levels dropped significantly, and they were found to absorb their thyroid medications (levothyroxine) more effectively than when they were consuming lactose.
This means that the consumption of dairy products can prevent thyroid hormones from working, while also causing an autoimmune attack on thyroid tissue.
The problem with pinpointing a dairy reaction, like all delayed food reactions, is that it’s almost impossible to know if dairy is a trigger for you, unless you go off dairy for at least two to three weeks, then reattempt eating it.
However, the good news is that, once the sensitizing food is eliminated for a few days to a few weeks, most people find that they feel better with less bloating, less acid reflux, normal bowel movements, more energy, etc. If we then consume that same food, the body will actually produce a stronger, more specific reaction, allowing us to recognize which particular food is problematic.
This is known as an elimination diet and is the gold standard for food-sensitivity testing.
If you think dairy may be a problem for you, I recommend removing it from your diet for at least two to three weeks and noting which symptoms are relieved for you.
Going dairy free helped 79 percent of people I surveyed – and it could be the one thing that can make a huge impact on your health, too.
Improvements that were reported by going dairy free included improved mood (46 percent), energy (54 percent), weight (41 percent), skin (37 percent), and pain (39 percent).
Less than two percent of people surveyed reported feeling worse by removing dairy, while 34 percent saw no noticeable difference.
Read more about Hashimoto’s and dairy.
4. Ditch the Sugar
Sugar is another commonly reactive substance found in Hashimoto’s.
Of the people that I surveyed, 87 percent reported feeling better when they ditched the sugar from their diet… so removing sugar from your diet may be something to try!
Are you hesitant to do so? I get it. In my past life, I would put three teaspoons of white, refined sugar in my tea. My brother would look at me in disgust and say, “This stuff will make you sick, Izabella. You need to cut out the sugar.”
I knew he was right — sugar can contribute to a yeast overgrowth, lowered immunity, weight gain, diabetes, and a whole host of health problems. Furthermore, it can contribute to blood sugar imbalances, which in turn can lead to inflammation and adrenal dysfunction (more on that later in this article) — but I was a sugar addict, and it was devastating to think that I would have to let go of this old friend and not have any sweetness in my life.
Fortunately, I eventually managed to wean myself off of sugar using a variety of substitutes (I started adding a teaspoon of myo-inositol into my tea). These days, I don’t crave the sweetness nearly as much as I used to, and many of my symptoms — including blood sugar balances that led to extreme fatigue — have been ditched along with the sugar!
Of the people with Hashimoto’s who took my survey, 65 percent saw improvements in their mood, 67 percent experienced more energy, 52 percent reported positive weight changes, and 29 percent improved the condition of their skin.
Less than two percent reported feeling worse after removing sugar from their diets, while 12 percent saw no noticeable improvement.
Removing refined cane sugar from your diet can be made easier with the many alternatives on the market. These include stevia, honey, molasses, maple syrup, coconut sugar, trehalose, xylitol, erythritol, monk fruit, and myo-inositol (among others). Take a look at my article on stevia for more information on sugar alternatives.
A word of caution, however: while natural sugar options are less toxic to our livers and contain beneficial nutrients, they are still high on the glycemic index and should be used sparingly to avoid sharp spikes in blood sugar. At the same time, while calorie-free sweeteners such as stevia and sugar alcohols (erythritol) won’t affect blood sugar levels, some people find that they are hard on the gastrointestinal system.
Unrefined cane sugars, which include sucanat, panela, rapadura, and muscovado, are sometimes used as healthier alternatives to refined sugar. However, while they do contain higher levels of nutrients such as calcium, potassium, magnesium, vitamin A and B vitamins, the sucrose levels are so high that they will still have a significant impact on blood sugar levels.
Instead, I encourage you to start weaning your taste buds away from sweets where possible.
Most people do find that, once they start reducing the level of sugar or sweetened foods and beverages that they consume on a daily basis, their cravings for those sweetened flavors fade, and they no longer miss the sweetness.
5. Eat a Low Glycemic Index Diet and Balance Blood Sugar
When we consume large amounts of sugar — often in the form of high carbohydrate foods such as desserts, grains, and starchy vegetables — the pancreas has to release larger amounts of insulin to bring the levels of sugar in the blood back down. These surges in insulin can cause blood sugar levels to drop too low, which then causes cravings for more carbohydrate-rich foods. This starts the cycle all over again as blood sugar levels swing high and low, creating stress in the body.
Common symptoms of blood sugar levels that are out of balance include hormonal issues, fatigue, depression, anxiety, insomnia, poor brain function, and chronic pain.
Blood sugar levels and the thyroid are intimately connected. In fact, one study that reviewed the current literature on the relationship between thyroid dysfunction and metabolic disorders, highlighted the fact that patients with diabetes were up to three times more likely to develop a thyroid disorder.
This correlation is due in large part to the fact that increased stress to the body will cause damage to the thyroid. When blood sugar levels are constantly fluctuating, the body experiences it as chronic stress. When the adrenals (the glands that are responsible for releasing stress hormones) become stressed, they release an excess of the hormone cortisol, which can also lead to an increased production of inflammatory proteins that are associated with a heightened immune response. This pattern eventually leads to an altered release of cortisol, which can, in turn, lead to numerous symptoms, including chronic fatigue, mood swings, and increased thyroid antibodies. (Weakened adrenals can also weaken the thyroid!)
Stabilizing blood sugar is an important part of protecting your adrenals from excess stress and healing from hypothyroidism. Improvements in mood, energy, brain function, and weight are positive side effects of proper blood sugar balance.
Focusing on the impact of food on our blood sugar is the most effective way to balance your blood sugar levels, and this is best accomplished by paying close attention to the glycemic index of foods.
The glycemic index is a measure of how quickly food becomes assimilated into our bodies. It can also be referred to as the “burn” rate — how quickly we burn the fuel we receive from these foods. Focusing on low glycemic index (GI) and low glycemic-loaded (GL) foods, which burn slower, can really help with balancing blood sugars.
Foods with a glycemic index above 55 are considered high glycemic index foods and include processed grains, sugar, starchy vegetables like potatoes, and sweet fruits like watermelon. For reference, refined sugar is scored as 61 (on a scale of 0-100) on the GI.
A low glycemic index diet helped 70 percent of those with Hashimoto’s.
Specifically, people who went on a low glycemic index diet reported improved mood (61 percent), energy (71 percent), and weight (53 percent).
Less than three percent of people surveyed felt worse on this type of diet, while 22 percent didn’t notice a difference in their symptoms.
For more information about the low glycemic index diet and blood sugar imbalances, please check out my article on the topic.
6. Supplement with Vitamin B12
Vitamin B12 is an essential water-soluble vitamin that is commonly found in animal proteins such as fish, shellfish, meat, eggs, and dairy products. B12 is required for protein synthesis, cell reproduction, and normal growth.
The risk for vitamin B12 deficiency is higher with increased age. It has also been found to be more prevalent in males and in people of Caucasian and Latin American descent. It results from insufficient intake, malabsorption from food, and other medical conditions that may prevent absorption.
In the case of people with thyroid disorders, a B12 deficiency is often a result of damage to the digestive tract that prevents the absorption of vital nutrients.
Another risk factor for B12 deficiency is small intestinal bacterial overgrowth, commonly known as SIBO, which may be present in up to 50 percent of people with Hashimoto’s.
Low levels of hydrochloric acid, commonly found in those with Hashimoto’s, also put people at risk for B12 deficiency. (This is because B12 is released for absorption with the help of hydrochloric acid, or stomach acid, and protease, an enzyme in the stomach.)
Because vitamin B12 is only found in animal proteins and not in plant foods, those that have been following a vegetarian or vegan diet are at an especially high risk for developing a B12 deficiency. Taking a vitamin B12 supplement is essential for vegans, and may be helpful for those with low stomach acid until the condition is corrected.
If you have a thyroid disorder, there is a very good chance that you are not absorbing B12, even if you eat a diet rich in animal proteins. You can test your levels, but please note that the consumption of bread and cereals fortified with folic acid (synthetic folate) may mask this deficiency on standard lab tests.
Along with removing problematic foods and supplementing with Betaine with Pepsin to restore healthy gut function, adding in a B12 supplement may go a long way to restoring your energy, cognitive function and overall sense of well-being.
Options for B12 supplementation include tablets, sublingual (under the tongue) liquids, and injections. I prefer the sublingual route, as there may be advantages for those with absorption issues, and it is more convenient than injections.
Sublingual doses of 5 mg (5000 mcg) of B12 daily for ten days, then 5 mg once per week for four weeks, then 5 mg monthly, have been found to be effective in restoring B12 levels in those with a deficiency.
Pure Encapsulations B12 comes in a convenient liquid form that can be administered sublingually for optimal absorption. The active form of B12 in this formulation is highly bioavailable and has been shown to support neurological function, nerve cell health, healthy cognitive and nerve function, as well as memory and emotional well-being.
In my survey of people with Hashimoto’s, 76 percent said they felt better after taking a B12 supplement.
Symptoms that saw the most improvement included energy (88 percent) and mood (56 percent). Only two percent of people surveyed said they felt worse while taking a B12 supplement, and 22 percent said they didn’t notice any changes.
Read more about the thyroid and B12.
7. Eliminate Grains
There are numerous dietary protocols that can help a person with Hashimoto’s feel better. In some cases, a dietary approach can produce a complete remission of the condition! These include the Specific Carbohydrate diet, Paleo diet, Autoimmune Paleo diet, low-FODMAPs diet, and Body Ecology diet, as well as gluten, soy, dairy, and iodine-free diets.
The connecting thread behind these diverse diets is that they all remove various reactive foods. Most of the diets also include animal proteins, are more nutrient dense than the Standard American Diet (S.A.D.), and remove processed foods.
There is no one-size-fits-all diet that will work for everyone with Hashimoto’s, and each person will need to individualize their diet to their own specific needs.
However, 81 percent of the people with Hashimoto’s who took my survey, felt better on a grain-free diet.
Grains are a highly processed food that is not easily digested by humans and can lead to many gastrointestinal issues, and even autoimmunity itself. These can include rice, millet, buckwheat, oats, bran, barley, wheat, corn, kamut, amaranth, spelt, and rye (among others).
Wheat, and even gluten-free products made with grains like rice and corn, can wreak havoc on our blood sugar. Amylopectin A, a complex carbohydrate in grains, is rapidly digested. This raises blood sugar higher than table sugar!
Grains also contain chemicals called phytates that block the absorption of important minerals such as calcium, magnesium, zinc, and iron. One in four individuals in the general population may be zinc deficient, and most people with hypothyroidism are, in fact, zinc deficient.
Grains are also acid producing, causing inflammation and a net acid load that may promote bone and muscle loss, as well as increase the risk for other health issues.
Of the people that took my survey, symptoms that improved by eliminating grains included energy (65 percent), mood (59 percent), weight (54 percent), and pain (44 percent).
Less than one percent of people reported feeling worse after eliminating grains, while 19 percent saw no difference.
To help determine if grains may be causing some of your symptoms, I recommend starting with an elimination diet, where you will eliminate grains for a period of time and keep track of how you are feeling.
Check out my articles on the Paleo and Autoimmune Paleo diets, as well as the Best Diet for Hashimoto’s, for more information on whether giving up grains might be right for you.
8. Incorporate Omega-3 Fatty Acids
Essential fatty acids (EFAs) are naturally occurring fats that the body cannot produce, therefore they are essential. They must be derived from either whole foods (like fish) or supplements.
EFAs help manage inflammation and autoimmunity, promote blood vessel health, support healthy skin growth, provide the precursors to balance hormones, and support healthy brain and nervous system function. They are considered essential because our bodies need them for so many reasons.
There are only two EFAs:
- linoleic acid (LA), an omega-6 fatty acid
- α-linolenic acid (ALA), an omega-3 fatty acid
There are also two types of omega-3s:
- eicosapentaenoic acid (EPA)
- docosahexaenoic acid (DHA)
The body requires about a 1:1 ratio of essential omega-3 and omega-6 fats for proper immune function and all the other roles EFAs play. Today, the average person on the Standard American Diet (S.A.D.) eats a ratio of as high as 25:1, with way too many omega-6 fats compared to omega-3 fats.
This can be a problem because omega-3 fatty acids reduce inflammation, while omega-6 fatty acids can promote inflammation. Inflammation serves a protective role in our bodies when the immune system is in balance, but in excess (as it is with autoimmune conditions), it can be problematic.
Many of us, especially those on the Standard American Diet, get too many omega-6 essential fatty acids and not enough omega-3 essential fatty acids, because we consume meat from animals fed grain, soy, and other foods that are not part of their natural diet. Even the healthiest diet will contain some omega-6s, but they should be nowhere near the amount many people consume. Grain-fed meats (including farm-raised fish) are big culprits.
Additionally, many of the oils in processed foods — including sunflower, cottonseed, soybean, sesame, and canola oils — provide high doses of omega-6s. Due to their role in immune function, omega-3 fatty acids are especially important for anyone with an autoimmune disease like Hashimoto’s. In fact, many autoimmune diseases are characterized by a high level of interleukin 1 (IL-1) and the pro-inflammatory leukotriene LTB(4), produced by omega-6 fatty acids.
While taking omega-3 acids in the form of fish oil or cod liver oil has been found to be helpful in a variety of autoimmune conditions, few studies have directly focused on the benefits of fish oil for thyroid issues and Hashimoto’s. One rodent study did find that a long-term diet rich in omega-3 EFAs lowered serum triglycerides and cholesterol while enhancing thyroid hormone signaling pathways in the liver.
Other conditions that fish oil has been shown to benefit include oxidative stress, pain management, brain health, depression, skin issues, gut health, adrenal health, and liver toxicity.
In fact, 76 percent of the people with Hashimoto’s whom I surveyed said that fish oil helped them feel better.
Improvements noticed by those who incorporated omega-3 fatty acids into their diet included mood (53 percent), energy (50 percent), skin 38 (percent), and hair 26 (percent).
While fresh fish can be an excellent source of omega-3 fatty acids, those with Hashimoto’s should use caution when consuming increased amounts of fish. Numerous studies (including the National Health and Nutrition Examination Survey or NHANES) have concluded that eating fish is the primary driver of elevated levels of mercury in the body.
Grass-fed meats also include a good amount of these omega-3 fatty acids, and freshly ground flaxseeds, chia seeds, and walnuts are great sources of ALA. However, it’s important to note that nuts and seeds are often food sensitivities for those with Hashimoto’s.
For that reason, the easiest and most effective way to get sufficient and balanced levels of ALA, EPA and DHA is to take a fish oil supplement.
Look for a professional quality fish oil supplement that has been molecularly distilled and filtered, such as EPA/DHA Essentials by Pure Encapsulations or OmegAvail™ Synergy by Designs for Health. This process ensures purity and helps eliminate contaminants including heavy metals, pesticides, solvents, and PCBs. Cod liver oil is another option that combines EPA and DHA with vitamins A and D.
Read my article on omega-3 fatty acids for more helpful information.
9. Optimize Vitamin D Levels
Vitamin D is an essential nutrient and a precursor hormone that plays an important role in many biochemical functions within the body. The body produces vitamin D from cholesterol, when our skin is exposed to sunlight. Vitamin D is also found in certain foods, such as fatty fish and fortified dairy products. However, it is very difficult to get adequate amounts through diet alone.
Do you ever feel worse in the winter than you do in the summer? A deficiency in vitamin D and a certain spectrum of light may hold the key to feeling better.
An estimated 85 percent of Americans may be deficient in it.
Autoimmune conditions are more likely to cluster in regions farther from the equator, and scientists have suggested that one of the potential reasons for this may be due to inadequate vitamin D levels, as vitamin D is primarily absorbed via sunshine on skin that is free of sunscreen.
Although those who live in warm climates are more likely to be absorbing enough of the sunshine vitamin, I often find that even people who live in warm climates are vitamin D deficient.
This is because our absorption of the vitamin from food sources is minimal, and is often further compromised by digestive enzyme deficiencies and gut conditions that lead to malabsorption of nutrients (such as infections and bacterial overgrowth).
While it is estimated that 1 billion people worldwide have low levels of vitamin D, most don’t realize that they’re deficient, as symptoms are often subtle. Indications that you may have a vitamin D deficiency include:
- Fatigue
- Bone aches
- Back pain
- Muscle pain and weakness
- Stress fractures (especially in your legs, pelvis, and hips)
- Frequent illness or infections
- Depression
- Impaired wound healing
- Osteoporosis
- Hair loss
Additionally, in those with Hashimoto’s, elevated thyroid antibodies may be a sign of a vitamin D deficiency.
One study in Turkey found that 92 percent of Hashimoto’s patients were deficient in vitamin D! In recent years, numerous studies have come out connecting vitamin D deficiency with the development of thyroid antibodies. The lower the vitamin D levels, the higher the thyroid antibodies.
When I surveyed my readers with Hashimoto’s, I found that 68 percent of them reported being diagnosed with vitamin D deficiency.
So how can we get adequate amounts of vitamin D?
Vitamin D can be produced in the skin when exposed to sunlight, or it can be ingested from foods and supplements.
One of the best ways to restore optimal vitamin D levels is through sun exposure. (As a bonus, sunlight has natural immune modulating benefits, and can also lift your mood.)
We can get vitamin D from dietary sources, including wild salmon (which contains 800 IU of D3 per 3.5 oz), cod liver oil (700 IU per teaspoon), fish, fortified dairy products and orange juice, and eggs.
However, the amount of vitamin D we absorb from food is limited, and people with fat malabsorption, food sensitivities, and other digestive issues common in Hashimoto’s, may be further impaired in their ability to absorb nutrients. Additionally, dairy, eggs and sugary drinks can be problematic for people with Hashimoto’s and blood sugar issues, so I don’t recommend relying on these foods for adequate vitamin D. This is why supplementation can be incredibly helpful, and why I recommend vitamin D supplements for most people with Hashimoto’s.
As the recommended daily allowance of 400 IU of vitamin D has been shown to be inadequate for most people, I generally recommend 5,000 IU per day as a starting point for my clients with Hashimoto’s. Taking your vitamin D supplements with a meal can be helpful in increasing its absorption by 30-50 percent.
However, I also recommend monitoring vitamin D levels to ensure that levels are within the optimal range (60 to 80 ng/mL for optimal thyroid receptor and immune system function).
The vitamin D supplements I recommend include:
- Pure Encapsulations Vitamin D 5000 IU (without vitamin K)
- Designs for Health Vitamin D Supreme (with vitamin K)
In my survey, 67 percent of my readers reported their fatigue improved and said they felt significantly better after taking a vitamin D supplement. (Less than 2 percent felt worse, and 24 percent reported no changes.)
Improvements in mood (64 percent), pain reduction (19 percent), as well as a reduction in antibody titers (35 percent), are also things I see time and time again.
Read more about thyroid and vitamin D.
10. Try the Paleo Diet
I often get asked, “What is the right diet for people with Hashimoto’s?”
As mentioned earlier, there is no single “perfect” diet that will work well for everyone, as we are all impacted by our unique genetics and environmental factors.
The best diet for any given person will depend on what food sensitivities they have, as well as if they’re having issues with blood sugar, undergoing chronic stress, or dealing with infections or toxin exposures. Additionally, how your body interprets those safety signals will depend on your gut health and your ability to digest and absorb key nutrients. It is very individualized.
While there isn’t a single perfect diet, there are elements of a perfect diet that do work well for most people, and those include:
- Removing triggering/reactive foods
- Eating healing foods
- Replenishing nutrients
The cavemen from the Paleolithic era actually seem to have gotten much of this right. Their diet was very focused on nutrient dense foods. Furthermore, they didn’t consume triggering foods (they didn’t have pesticides, antibiotic and hormone-laden foods, and GMOs; nor did they have gluten, refined grains, or other processed foods!). Their diet has inspired Paleo diets that have become popular today.
The historical theory behind the health benefits of a Paleo diet is that the digestive systems of humans have not had sufficient time to adapt to today’s farming practices or to the ingredients and chemicals in modern processed foods. (The theory blames the rise in chronic diseases, obesity, and allergies on the agricultural revolution which added grains and processed foods — and toxins — into our diet.)
In other words, our genetics have pre-programmed us for optimal health if we eat our ancestors’ food choices. So, the foods allowed on a Paleo diet are based on what historians think our pre-agricultural, hunter-gatherer cavemen ancestors ate.
It is estimated that contemporary Western populations get as much as 70 percent of our daily energy intake provided by foods that were never or rarely consumed by our hunter-gatherer Paleolithic kin. These non-Paleo-compliant foods include grains, refined sugars, dairy, soy, legumes, and highly processed fats.
A Paleo diet replaces these with nutrient-dense foods thought to have been eaten during the Paleolithic era: nuts and seeds, vegetables, fruit, and eggs. Meat, a caveman staple, is also allowed, as is fish and other meat products (organ meats).
The Paleo diet not only removes reactive foods but focuses on many healing foods with significant nutritional benefits, providing:
- Nutrient density
- Controlled blood sugar levels and glucose tolerance
- More disease-fighting omega-3 fats
- Less inflammation
- Lots of dietary fiber
Of those surveyed, 81 percent reported feeling better on a grain-free or Paleo diet.
Corn, in particular, was noted as a large sensitivity, as was gluten. Other food triggers included dairy (79 percent of respondents felt better, and dairy was a large sensitivity for me!), eggs (48 percent), sugar (87 percent), and soy (63 percent).
If you’ve found a lot of the dietary interventions in this article resonate with you so far, and you’re ready to ditch the gluten, grains, dairy, and sugar, you might want to take the next step and try a Paleo type of diet.
Of those who took my survey, 71 percent noticed improved mood, 79 percent experienced more energy, and 60 percent reported positive weight changes on a Paleo diet.
I’ve actually tweaked the standard Paleo diet guidelines a bit based on my clients’ successes. I call my diet the Root Cause Paleo Diet, and you can read more in-depth information on this diet — and other diets — in my article titled The Best Diet for Hashimoto’s.
You can also read more about the Paleo diet and Hashimoto’s in my article.
To help get you started, I have a wonderful recipe guide that can help jump-start your Paleo diet today. You can download my free Paleo recipe guide here.
The Takeaway
While there are many interventions that can help a person with Hashimoto’s get into remission and feel better, the ten mentioned in this article have been some of the most effective ones for my readers, and have resulted in tremendous improvement. Additionally, they are all easy to implement, low-cost (sunshine is free!), and don’t require a doctor’s prescription.
Other interventions that have shown to be effective include using turmeric, advancing to the Autoimmune Paleo diet, and taking liver support supplements.
For a comprehensive guide on how to take your thyroid health into your own hands, including a step-by-step program for implementing many of these interventions, I encourage you to pick up a copy of my book Hashimoto’s Protocol.
I hope that you found this information helpful in your healing journey!
P.S. Be sure to sign up to my email list to get a free book chapter, recipes, Thyroid Diet start guide, notifications about upcoming events, and my weekly newsletter.
Be sure to follow me on Facebook and Instagram for more news, tips, and the chance to interact with our Hashimoto’s community!
References
- Valentino R, Savastano S, Maglio M et al. Markers of potential coeliac disease in patients with Hashimoto’s thyroiditis. European Journal of Endocrinology. 2002;146(4):479-483. doi:10.1530/eje.0.1460479.
- Skodje G, Sarna V, Minelle I, et al. Fructan, Rather Than Gluten, Induces Symptoms in Patients With Self-reported Non-celiac Gluten Sensitivity. Gastroenterology. 2017;S0016-5085(17):36302-36303. doi:10.1053/j.gastro.2017.10.040.
- Schnedi W, Lackner S, Enko D, Schenk M, Mangge H, Holasek S. Non-celiac gluten sensitivity: people without celiac disease avoiding gluten-is it due to histamine intolerance? Inflammation Research. 2017. doi:10.1007/s00011-017-1117-4.
- Leccioli V, Oliveri M, Romeo M, Berretta M, Rossi P. A New Proposal for the Pathogenic Mechanism of Non-Coeliac/Non-Allergic Gluten/Wheat Sensitivity: Piecing Together the Puzzle of Recent Scientific Evidence. Nutrients. 2017;9(11):1203. doi:10.3390/nu9111203.
- Köhrle J. The trace element selenium and the thyroid gland. Biochimie. 1999 May;81(5):527-33.
- Rybicka I, Krawczyk M, Stanisz E, Gliszczyńska-Świgło A. Selenium in Gluten-free Products. Plant Foods for Human Nutrition. 2015;70(2):128-134. doi:10.1007/s11130-015-0467-8.
- Mazokopakis EE, Papadakis JA, Papadomanolaki MG, et al. Effects of 12 months treatment with L-selenomethionine on serum anti-TPO Levels in patients with Hashimoto’s thyroiditis. Thyroid. 2007 Jul;17(7):609-12.
- Negro R. Selenium and thyroid autoimmunity. Biologics : Targets & Therapy. 2008;2(2):265-273.
- Stagnaro-Green A. Postpartum thyroiditis. Best Pract Res Clin Endocrinol Metab. 2004 Jun;18(2):303-16.
- Goyens P, Golstein J, Nsombola B, Vis H, Dumont JE. Selenium deficiency as a possible factor in the pathogenesis of myxoedematous endemic cretinism. Acta Endocrinologica. 1987;114(4):497–502.
- Levander OA, Beck MA. Interacting nutritional and infectious etiologies of Keshan disease: insights from Coxackie virus B-induced myocarditis in mice deficient in selenium or vitamin E. Biol Trace Elem Res. 1997;56:5–21.
- Blood Sugar Major Player in Hashimoto’s Hypothyroidism. Functional Health News Website. http://functionalhealthnews.com/2014/08/blood-sugar-chronic-health/. Accessed February 5, 2019.
- Ruchala M, et. al. The influence of lactose intolerance and other gastro-intestinal tract disorders on L-thyroxine absorption. Endokrynol Pol. 2012;63(4):318-23.
- Groth E. Fish Consumption and Blood Mercury Levels. Environ Health Perspect. 2014 May;122(5):A120.
- Souza LL1, Nunes MO, Paula GS, Cordeiro A, Penha-Pinto V, Neto JF, et al. Effects of Dietary Fish oil on Thyroid Hormone Signaling in the Liver. J Nutr Biochem. 2010 Oct;21(10):935-40.
- Tamer G, Arik S, Tamer I, Coksert D. Relative vitamin D insufficiency in Hashimoto’s thyroiditis. Thyroid. 2011;21(8):891-896. doi:10.1089/thy.2009.0200.
- Wang J, Lv S, Chen G, et al. Meta-analysis of the association between vitamin D and autoimmune thyroid disease. Nutrients. 2015;7(4):2485-2498. doi:10.3390/nu7042485.
- Vahabi P, Aminorroaya A, Amini M, et al. Effect of Vitamin D deficiency treatment on thyroid function and autoimmunity markers in Hashimoto’s thyroiditis: A double-blind randomized placebo-controlled clinical trial. Journal of Research in Medical Sciences : The Official Journal of Isfahan University of Medical Sciences. 2017;22:103. doi:10.4103/jrms.JRMS_1048_16.
Note: Originally published in May 2015, this article has been revised and updated for accuracy and thoroughness.



 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
This is such a great article. Thank you! Can you offer any suggestions for folks who experience gallbladder inflammation in response to eating meat? Thanks!
Jen – thank you for reaching out. <3 Here is an article you might find helpful:
HOW GALLBLADDER AFFECTS HASHIMOTO'S
https://bruno-michael-wentz.dev01.rmkr.net/articles/how-gallbladder-affects-hashimotos/
When I was at my lowest point, the challenge of radically changing my diet–when I was barely able to care for myself as it was–was too overwhelming to contemplate. My diet was not bad, but it certainly did include dairy and gluten, as it still does.
However, it’s worth pointing out that 4 of these 10 excellent suggestions require no more mental or physical effort than buying and opening a pill bottle: 1) Selenium, 2) Vitamin D, 3) Omega-3 fish oil, and 4) Vitamin B-12. After doing these 4 things (plus, I should add inositol, probiotics and sloooowly increasing amounts of exercise), I gradually found my energy and optimism significantly increased. (As did my body temperature.) After that it became a lot more manageable to consciously make changes to my diet, cutting even more refined carbs and adding more vegetables, 16 hour fasts (not for everyone, I know), and so on.
Pills alone might not be as effective for others, but for me they were a great help on the way to other more effortful improvements
Chicken Little – thank you so much for sharing what has worked for you! <3