If you have Hashimoto’s and you aren’t working on supporting your adrenals, you’ll want to read this!
I still remember when my integrative doctor suggested I get tested for adrenal fatigue after my Hashimoto’s diagnosis — I was skeptical. Like most conventionally trained healthcare professionals, I was only familiar with one kind of adrenal disease — Addison’s disease, which is a life-threatening condition where your adrenals don’t produce enough cortisol.
When I searched “Dr. Google,” I found that “adrenal fatigue” was considered a bogus “quack” diagnosis. I delayed testing my own adrenals for a long time. It wasn’t until I spoke with another pharmacist, Carter Black, RPh, about my lingering symptoms and he suggested adrenal testing that I decided to give it a try. Maybe I was more open to it because we had similar training and he wasn’t trying to sell me anything, or maybe the timing was just right.
Sure enough, the integrative adrenal test showed that I had an advanced stage of adrenal dysfunction. I followed the recommended protocols and saw incredible improvements in my energy levels, emotional state, blood sugar issues, and hormone balance — quickly!
Since then, I’ve experienced and overcome adrenal dysfunction two more times. All the while, I was helping many of my thyroid patients support their adrenals as well.
It’s been so fascinating to see how many people couldn’t fully resolve their thyroid symptoms until they addressed their adrenals. In my experience, it’s often the missing piece of the puzzle for many people with Hashimoto’s and thyroid issues.
The Adrenal-Thyroid Connection
The hypothalamic-pituitary-adrenal axis, otherwise known as the HPA axis, describes the interactive feedback loop that takes place between these three endocrine glands. (1)
The hypothalamus is like the CEO of our body’s production of hormones. It scans messages from our environment and other endocrine glands, as well as checks the body’s overall hormonal status, before passing on the order for more hormones to the pituitary gland. The pituitary gland then acts as a project manager and will pull together individual workers (like the thyroid gland, the adrenal gland, and the gonads) to do their jobs. The pituitary will also make sure the workers have adequate resources to do their jobs by managing growth and repair, as well as electrolyte/water balance.
In cases of immediate stress, the hypothalamus senses stress and sets off a hormone cascade that leads to the activation of our fight-or-flight response. As part of this response, the adrenals pump out extra hormones, and our bodies go from the state of relaxing, digesting, and healing, to a survival state.
Our body’s energy is shifted from activities not essential to survival, like growing beautiful hair, metabolizing nutrients into energy, making hormones, and digesting and repairing itself, to instead focusing its resources to meet the great, stress-induced demand for cortisol and adrenaline.
Then, once we’ve escaped from the threatening bear or gotten out of the way of the oncoming car, the demand for emergency levels of hormones settles down, and the focus once again turns to the parasympathetic response, focused on body maintenance and upkeep.
In cases of chronic stress, the never-ending presence of stressful, yet non-life-threatening, situations can lead to the constant activation of the stress response.
To help meet the demand for cortisol, your body will decrease the production of other hormones normally produced by the adrenals such as progesterone, DHEA, and testosterone. (2)
Eventually, with enough chronic stress, the HPA axis becomes overwhelmed and desensitized to the usual feedback loop, and stops sending messages to the adrenals to produce more hormones or less hormones, no matter what’s happening. (3)
This process directly affects the thyroid — high cortisol will slow down thyroid hormone production, meaning chronically elevated cortisol can have a big impact on thyroid function.
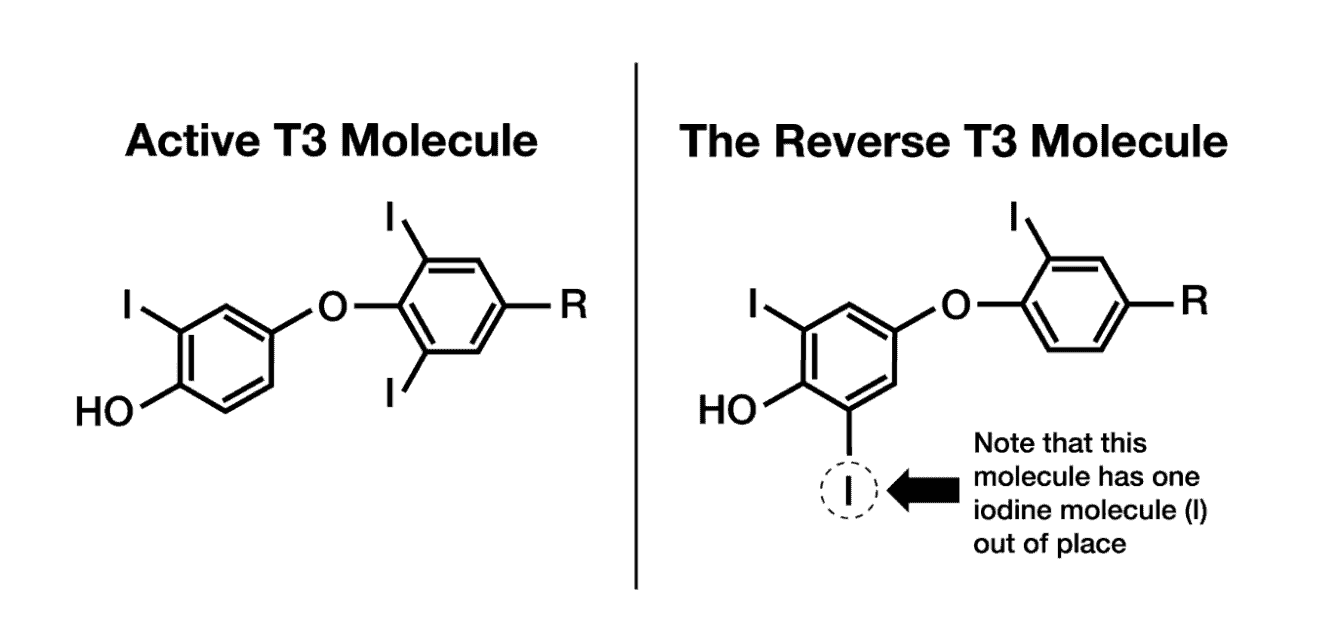
In the early stages, high cortisol increases antibody production and inhibits the peripheral conversion of T4, the inactive thyroid hormone, to T3, the active thyroid hormone.
At the same time, cortisol promotes the production of reverse T3 (rT3), an inactive thyroid molecule that is able to bind and block T3 hormone receptor sites. This prevents the necessary reactions needed for active thyroid hormone and leads to hypothyroid symptoms, despite adequate amounts of thyroid hormones and “normal” thyroid labs. Cortisol also prevents the release of TSH, halting the production of more thyroid hormones.
Additionally, hypothyroidism slows down the clearance of cortisol, and treating the thyroid without addressing adrenal dysfunction can accelerate the clearance of cortisol. When we do so, we may actually end up with low cortisol levels, and as we know, we do need certain levels of cortisol for energy and alertness.
Testing and Cortisol Patterns
The standard test for thyroid function is thyroid stimulating hormone (TSH), but there are a few problems and limitations with the TSH test. First, the conventional ranges for TSH are much too broad, with some ranges as lax as 0.2 to 8.0 μIU/mL. Many of my colleagues in the functional medicine community, as well as myself, have found that optimal reference ranges should be between 0.5 and 2 μIU/mL for a healthy adult not taking thyroid medications.
Another issue is that people’s TSH can remain normal for years, while they’re experiencing hypothyroid symptoms. This means that these people often go untreated, and without resources for their symptoms. This is why antibody tests are important, as people with Hashimoto’s often have elevated antibody levels for years before their TSH is abnormal. You can read more about my top thyroid tests here.
What about adrenal testing? I have been talking about the connection between adrenal dysfunction and hypothyroidism for quite some time, and unfortunately, I don’t think I have been clear enough.
People will come across the term “adrenal fatigue” and resonate with all the symptoms, so they’ll ask their conventional doctors to test them for adrenal issues. The doctors will test them for Addison’s disease (a rare, serious cause of adrenal insufficiency that can be life-threatening), and the tests almost always come out “normal.” That is because Addison’s is a disease where the adrenals are destroyed and unable to produce stress hormones, while adrenal dysfunction is an adaptive response to stress. In adrenal dysfunction, the adrenals are still capable of producing stress hormones, but there’s a disconnect between them and the signals to produce cortisol, at the right times of day in the right amounts, that are sent by the brain.
That said, there are ways to test for adrenal dysfunction. Two of my favorite tests are the adrenal saliva test and the DUTCH urine test.
Adrenal saliva tests can be ordered by integrative practitioners, but are considered “experimental” by conventional medicine, and thus, not usually covered by insurance. I used to use them quite frequently in my practice, and they helped me gain insight into the kind of cortisol issues most people with Hashimoto’s experience.
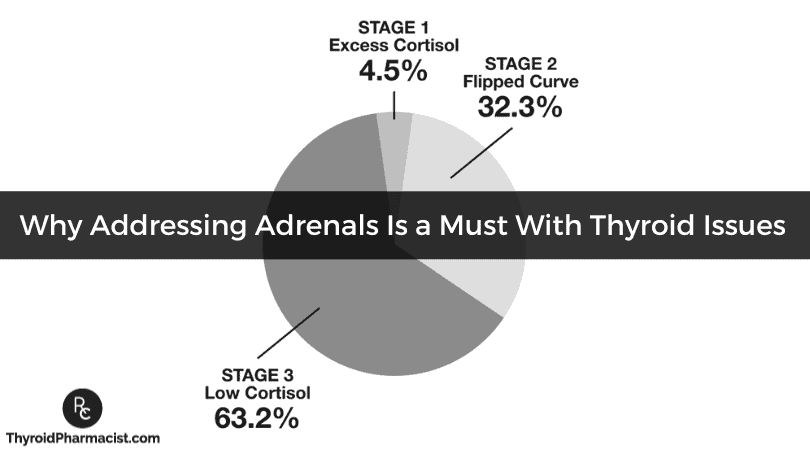
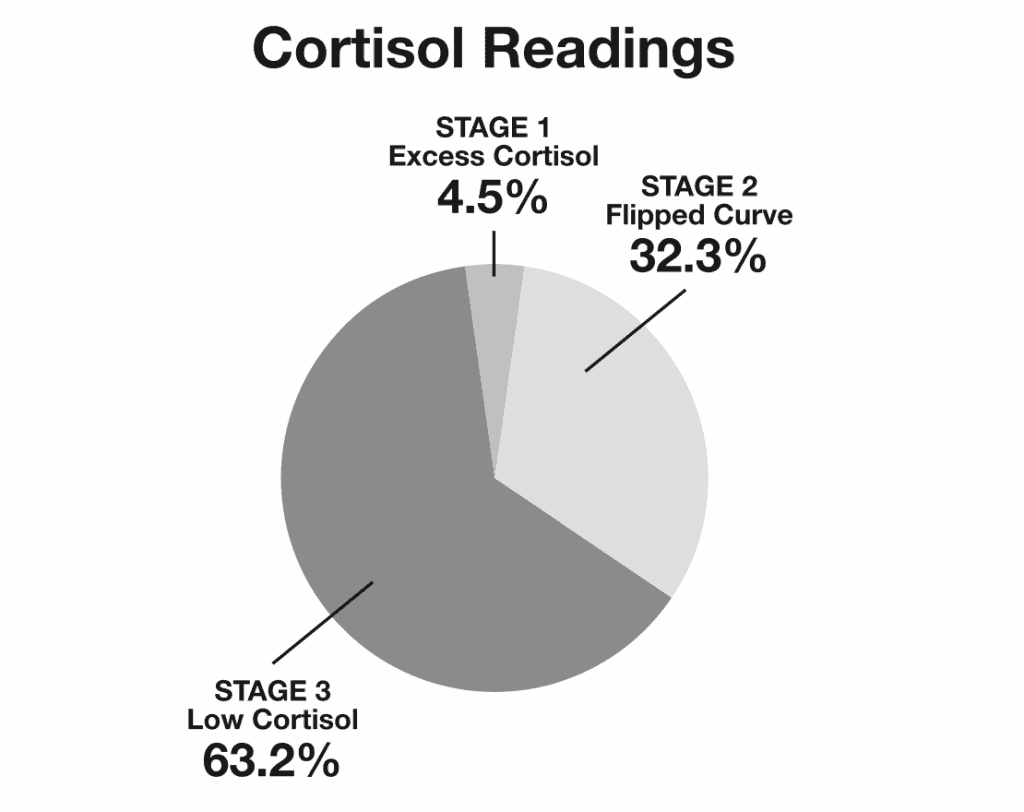
In analyzing 148 adrenal saliva tests of symptomatic people with Hashimoto’s from 2015 to 2019, I have noticed that all of the individuals tested had some degree of adrenal dysfunction.
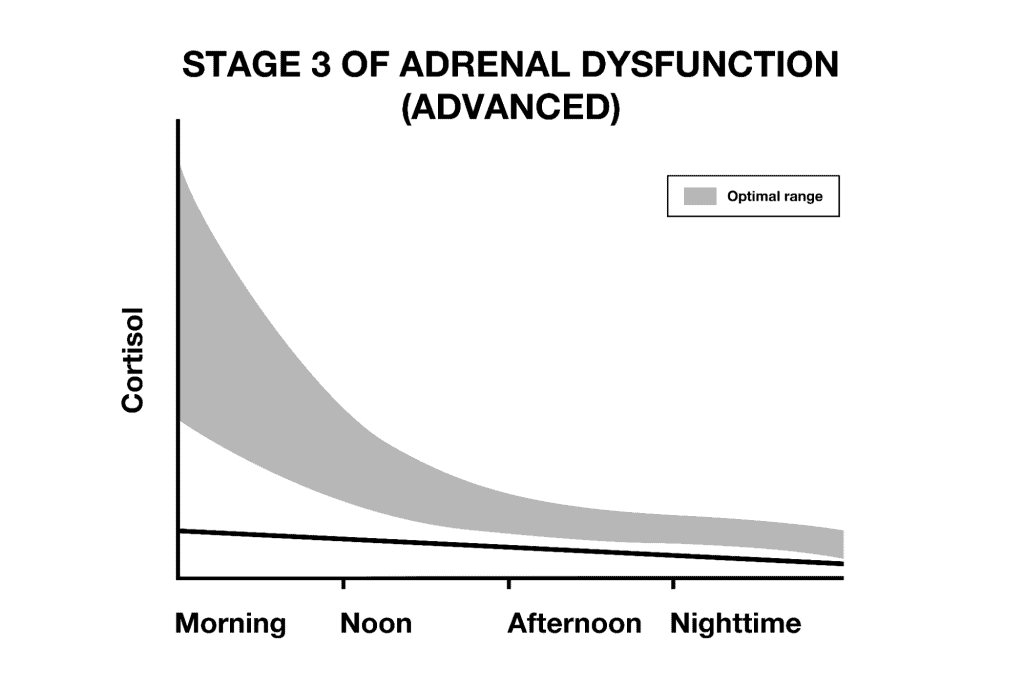
Optimally functioning adrenals are supposed to put out the most cortisol in the morning, and cortisol should decline gradually and smoothly during the day, until very little cortisol is secreted at bedtime. This helps people to be aligned with the circadian rhythm, so they have more energy in the morning, and are tired at night.
Adrenal saliva tests performed in healthy individuals align with this circadian release of cortisol.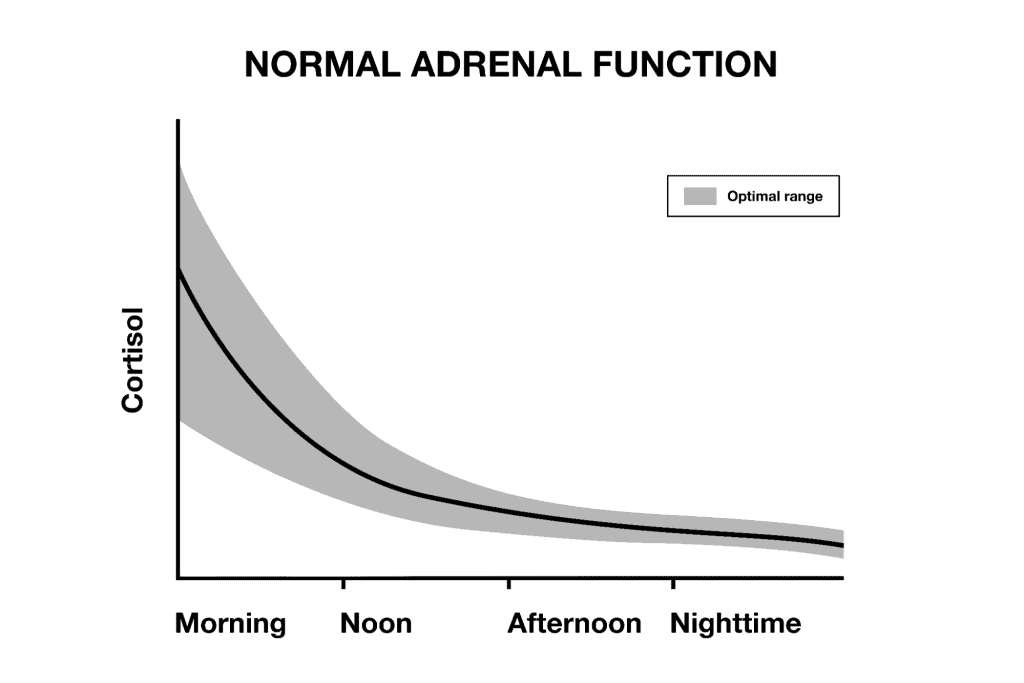
In stage 1 of adrenal dysfunction, we see elevated cortisol levels throughout the day, and even at night, which can leave people feeling anxious, irritable, and wired.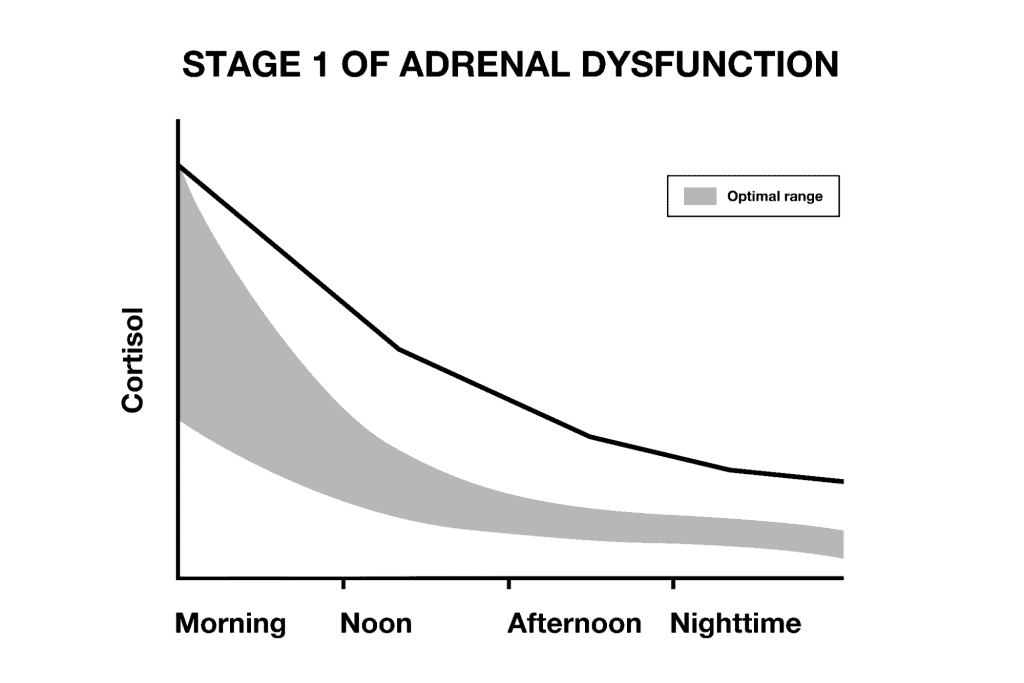
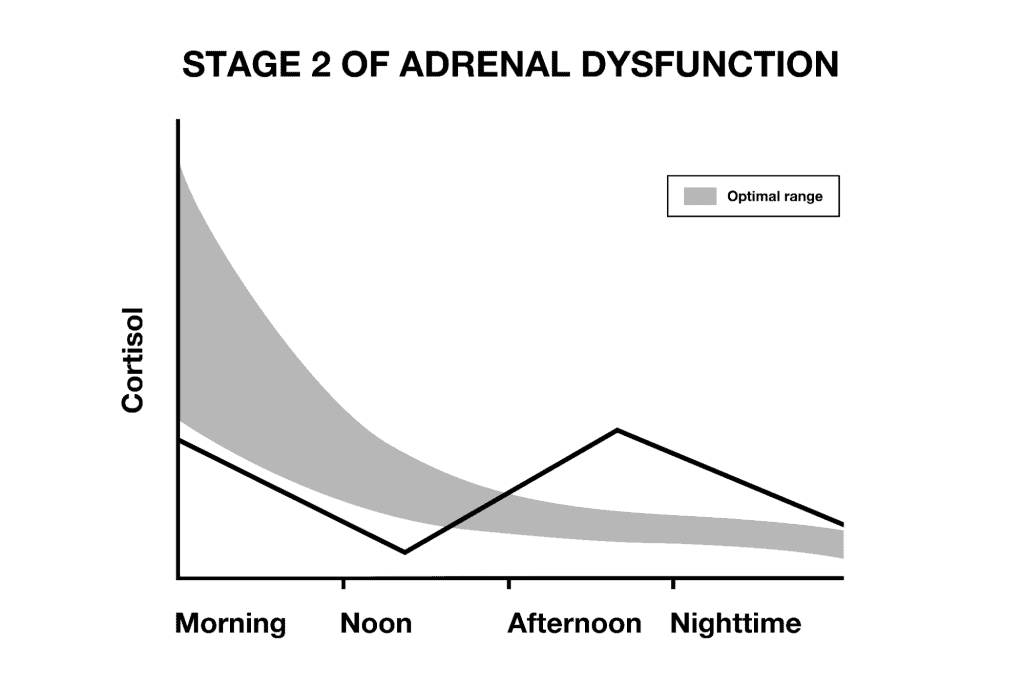
In stage 2, the communication breakdown between the brain and the adrenals starts to happen. The cortisol curve of someone in stage 2 of adrenal fatigue resembles a rollercoaster, with cortisol spiking and dropping at the wrong times. This person may be groggy in the morning, feel more energetic in the afternoon, then may experience anxiety or even a second wind in the evening.
Other individuals in stage 2, heading into stage 3, may present with low cortisol for most of the day, with a cortisol surge in the evening. This is the person that has a hard time waking up in the morning, is tired throughout the day, and doesn’t “wake up” until the evening (sometimes these are the “night owls”).
As time goes on, someone might progress to stage 3 of adrenal fatigue, where cortisol drops lower and lower. In stage 3, someone will feel chronically exhausted and may be dependent on caffeine to function.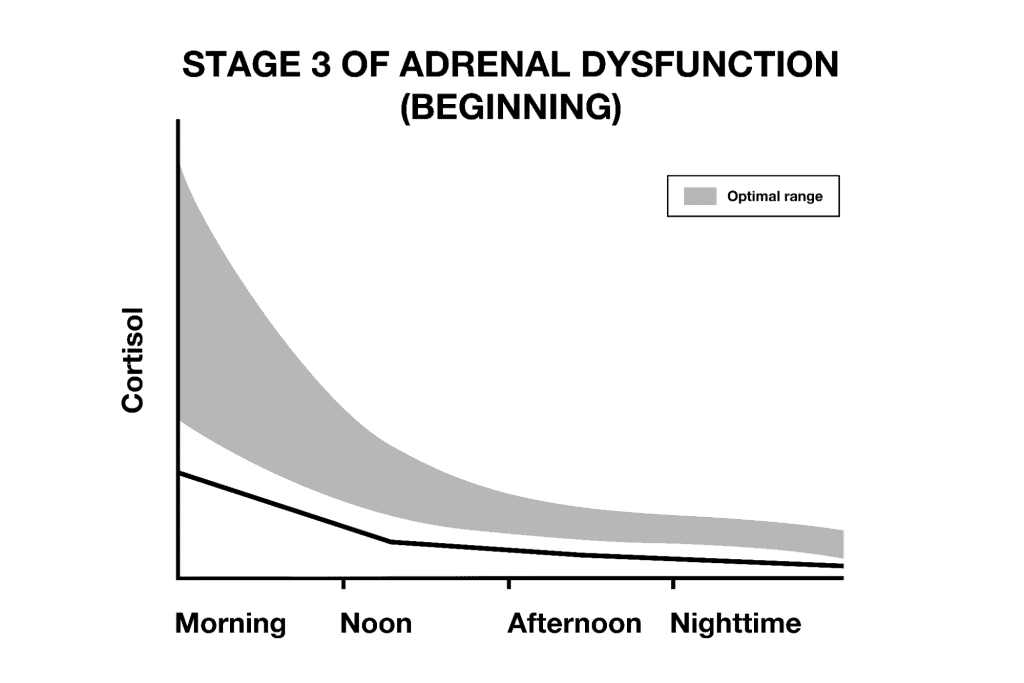
ADRENAL SALIVA PATTERNS IN SYMPTOMATIC PEOPLE WITH HASHIMOTO’S
We often hear about how cortisol is “bad,” and many of the recommendations you will see in mainstream media, and perhaps even from well-meaning healthcare professionals, focus on lowering cortisol.
Yet, out of the 148 tested individuals with Hashimoto’s, only 7 showed an excess of cortisol, while the majority (63.2% or 91 individuals) had low levels of cortisol.
Furthermore, there were 50 people whose cortisol was in the “normal” range but their cortisol curve was off, so they were producing either too little cortisol in the morning, they had fluctuations at their noon/afternoon readings, or they produced too much at night, leading to morning fatigue, midday mood swings, and/or trouble sleeping at night.
Over the years, I have noticed that these patterns of dysregulated cortisol can be consistently and accurately linked to symptoms.
For example, we see excessive fatigue, low blood sugar, and low blood pressure when low cortisol is present, and we see irritability, racing thoughts, high blood sugar, and high blood pressure when there are high levels of cortisol.
Unfortunately, many of the “cortisol-lowering” suggestions from mainstream media and even well-meaning healthcare professionals can make a person with low cortisol, or even normal cortisol, feel worse.
Why Don’t More Doctors Know About This?
The term “adrenal fatigue” has many conflicting messages surrounding it. On one side there are some professional medical organizations, such as the Endocrine Society, stating that “no scientific proof exists to support adrenal fatigue as a true medical condition,” and research published in reputable medical journals declaring that a systematic review of nearly sixty studies “proves that there is no substantiation that ‘adrenal fatigue’ is an actual medical condition. Therefore, adrenal fatigue is still a myth.” (4)
On the other side, there are well-known, respected functional, naturopathic, and integrative medical experts acknowledging its existence, explaining how it develops, and offering ways to treat it (including yours truly :-)).
To complicate the matter more, some integrative practitioners have now begun to say that adrenal fatigue is, in fact, a myth!
It seems to me that there’s a disagreement over word choice and the proposed physiology behind the cluster of real and frustrating symptoms. The term “adrenal fatigue” was first used by Dr. James L. Wilson in 1998 to identify below-optimal adrenal function resulting from stress. The thinking was that as the adrenals become overwhelmed by stress and excess cortisol release, they become unable to produce sufficient cortisol and other adrenal hormones.
Wilson’s new term was a useful way to describe a cluster of symptoms including fatigue, insomnia, and cravings for salty and sweet foods, among others. It also helped distinguish the condition from Addison’s disease (also known as adrenal insufficiency), a rare, life-threatening disorder in which the adrenal glands are unable to produce enough cortisol. Addison’s is usually caused by autoimmune damage to the adrenals, leading to similar but more extreme symptoms such as extreme fatigue, weight loss, darkening of the skin, low blood pressure, and low blood sugar.
As we’ve learned more about the body and how it responds to stress, we’ve realized that the original description of the mechanisms behind adrenal fatigue isn’t accurate. Most modern integrative practitioners recognize that the adrenals do not become “fatigued,” worn out, sleepy, tired, sluggish, or lazy because of chronic stress.
Instead, the newly proposed mechanism is that a communication breakdown between the organs of the HPA axis leads to an imbalance of adrenal hormones. The adrenal glands may be physically healthy and perfectly capable of producing adrenal hormones but, because of the communication breakdown, they may not be receiving the message to make them or may produce them at improper times.
The term “HPA axis dysfunction” (or “adrenal dysfunction”) is now the term that is used to describe the cluster of stress symptoms, as it more accurately describes what’s happening in the body. Additionally, the term “hypocortisolism” is used to describe the lowered production of cortisol.
Yet, conventional medicine continues to debate the narrowly-defined term “adrenal fatigue,” leading to those stunning oversimplifications that the condition does not exist.
Conventionally trained doctors utilize blood tests and occasionally imaging of the adrenals to look for certain adrenal gland disorders, such as Addison’s disease and Cushing syndrome (excessive production of cortisol from the adrenal glands) and the over- or underproduction of adrenal hormones due to nodules or tumors on the adrenals or pituitary gland, and are not well versed in the more broadly defined adrenal dysfunction. They will not utilize the urine and saliva tests used by functional practitioners, as those are usually not covered by insurance, and many people with stress-related symptoms are often told that all of their lab tests are normal, their symptoms are normal, or worse – that their symptoms are all in their head.
While I am so grateful for conventional medicine, it has its limitations when it comes to this gray area of adrenal dysfunction.
How Does Integrative Medicine Approach Adrenal Dysfunction?
When I first found out I had adrenal dysfunction, I decided to take a few practitioner courses, and I learned about various ways to modulate cortisol levels after reviewing test results that showed the patient’s cortisol pattern.
- Hormones, including pregnenolone and DHEA, can be used in a circadian fashion to mimic a healthy cortisol pattern throughout the day in an effort to “reteach” the body when to produce cortisol and how much to produce.
- Glandulars, extracts made from the adrenal glands of animals, can be used to give someone more adrenal hormones, usually in the mornings.
- Hydrocortisone, in small doses, can be prescribed for people with low cortisol.
- Licorice extract can be used to prevent the breakdown of cortisol and to raise cortisol levels in the mornings and afternoons.
- Phosphatidylserine can be used to lower cortisol, especially in the evenings, allowing for better sleep.
In addition to modulating cortisol levels, integrative practitioners often focus on lifestyle recommendations, such as getting more sleep, de-stressing, and quitting caffeine.
Adaptogenic herbs, B vitamins, and vitamin C are also recommended to support a healthy stress response.
A New Path to Heal the Adrenals
I’ve personally experienced three bouts of adrenal dysfunction.
While I successfully overcame the first two with the more traditional protocols of using hormones, sleeping for 10-12 hours per night, and cutting out caffeine, I found myself in a more challenging situation after the birth of my son. Around eight months postpartum, I found myself with a flatlined adrenal cortisol pattern, due to the sleep deprivation of being a new mom.
During this third bout of adrenal dysfunction, I couldn’t use my go-to protocols. There was no way I was getting 10-12 hours of sleep each night as a new mom, and there was no way I was giving up the caffeine that was so supportive to me during the day. I also wasn’t comfortable taking hormones, which I had done in the past, because I was still breastfeeding.
I knew there had to be another way! I dove deep into various healing modalities and started focusing on sending my body “safety signals” that helped me to align with the circadian rhythm, get more restful sleep, and replenish the nutrients that are often lost during stressful times. Within a few short weeks, I was able to not only reverse my adrenal dysfunction, but also thrive as a new mom!
I was so thrilled to have discovered a protocol that was not only effective but also gentle and easy to adhere to, as it doesn’t use hormones to boost or suppress cortisol levels. Since my protocol focuses on circadian realignment, which has a normalizing effect on overall cortisol levels, this protocol can be used by people with low OR high cortisol. Furthermore, adrenal testing is not required, as the protocol focuses entirely on your symptoms!
Over the last decade, I have become really attuned to listening to the body’s subtle cues as to what is out of balance, and I hope to teach you to do the same.
I started recommending this protocol to my clients, and in 2020 I introduced my Adrenal Transformation Program to my community!
The program delivered mind-blowing results to participants, and most of them started feeling better in as little as three weeks. These are some of the improvements that participants experienced:
- 92% had reduced mental fog
- 89% reported reduced fatigue
- 89% reported reduced forgetfulness
- 86% reported reduced anxiety
- 85% felt less irritable
- 81% experienced less trouble sleeping
- 81% improved their libido
- 78% reduced feelings of depression
- 76% reduced their joint pain
Over 3,000 people have now been through the program and continue to see amazing results.
Here’s what Natasha had to say after going through the program:
“I felt like I did over 10 years ago! I’m 57 and I’ve had the energy that I had when I was 27!! I’ve been doing tons of work outside (like trimming bushes and weeding—all things I had not been able to do because my joints would hurt so much) and I feel great! No pain. No loss of energy. No need to sleep the next day to recover! My husband has been telling the kids that he can’t keep up with me! It used to be the other way around!”
And Mariana is thriving:
“I loved this course. . . . I followed the protocols and feel significant improvements. The brain fog has lifted! My memory has improved. I have less muscle pain, particularly after exercise. I have more energy and better sleep. I handle stress better. I lost weight. What is most important, I feel great!”
I wanted to create a way for this program to reach more people, as stress continues to increase in our modern world, and I know so many people are struggling with fatigue, brain fog, and mood issues, and not finding the help they need. This is why I decided to put my tried and true program into book form, so that it can reach more people
That is how my newest book, Adrenal Transformation Protocol, was born. In it, you’ll find a simple four-week program to help you balance your stress response and gradually build up your resilience, to prevent excess stress from overwhelming your adrenals. Adrenal Transformation Protocol will set you up with a strong foundation to return to and stay in homeostasis through turbulence.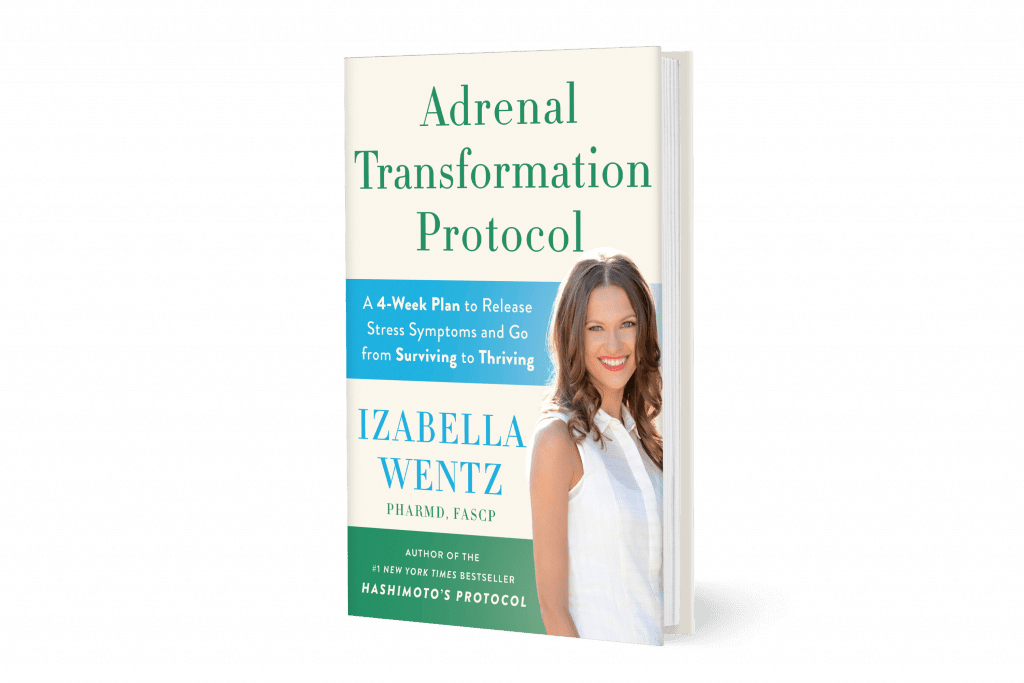
This book is for anyone experiencing brain fog, fatigue, sleep issues, chronic pain, low libido, and/or mood issues. If you have come to a healing plateau in your thyroid journey, or are looking for a way to become more resilient in the face of all the stress life throws at you, this book can truly transform your health!
The body communicates to us through symptoms, and Adrenal Transformation Protocol focuses on giving you a comprehensive plan to rewire your stress response, as well as a detailed back section to teach you how to understand and address your symptoms, including brain fog, fatigue, sleep issues, anxiety, low libido, and pain.
If you know something is “off” despite normal lab tests, or if you’re having trouble finding resources and support for adrenal dysfunction, then this book is for you!
When we start supporting the adrenals — making a few small dietary and lifestyle changes and taking the right supplements — we can produce profound improvements in energy levels, feel calmer, and allow our body to repair itself, within weeks or even days. You can get a new lease on life and feel like yourself again in just a few short weeks!
I’m so excited to share this book with the world. You can order your copy now!
For future updates, make sure to follow me on Facebook, Instagram, TikTok, and Pinterest!
P.S. Would you take a moment and share this information with anyone who you think might benefit from it? I’m on a mission to spread hope and help as many people as I can!
References
- Cook SB. Current Controversy: Does Adrenal Fatigue Exist?. Natural Medicine Journal. 2017;9(10).
- Mariotti A. The effects of chronic stress on health: new insights into the molecular mechanisms of brain-body communication. Future Sci OA. 2015;1(3):FSO23. Published 2015 Nov 1. doi:10.4155/fso.15.21; Harvard Health Publishing. Understanding the stress response. Harvard Health Publishing. https://www.health.harvard.edu/staying-healthy/understanding-the-stress-response. Published March 2011. Updated March 18, 2016. Accessed February 25, 2018.
- Cook SB. Current Controversy: Does Adrenal Fatigue Exist?. Natural Medicine Journal. 2017;9(10).
- Adrenal fatigue. Endocrine Society. https://www.endocrine.org/patient-engagement/endocrine- library/adrenal-fatigue. Published July 7, 2022. Accessed March 24, 2023.


 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
I have read many of your articles and they seem to be geared toward Hashimoto’s hypothyroidism. Do you have any informational articles or blogs pertaining to hypothyroidism due to papillary cancer with total thyroidectomy?
The other day I was doing some research and I was shocked to discover that hypothyroidism and frozen shoulder had a connection. My thyroid was removed in 2010 and I had RAI 131. About 4 or 5 years ago I discovered I have frozen shoulder syndrome and it hurts. Two years after that I now have it in my right shoulder. I am amazed and shocked by what the lack of a thyroid can cause even with medication.
Would appreciate any help you can provide.
Rhonda – thank you for reaching out. I do not have an article at this time. I’m so sorry ou have been through all of this. Removing the thyroid with a thyroidectomy eliminates thyroid antibodies, as there is nothing left to attack. However, life is not always roses with a thyroidectomy, as it does not remove the autoimmunity. Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Even when the thyroid is taken out surgically or treated with radioactive iodine the autoimmunity still persists in most cases. Many people will have their thyroids removed, and will develop new autoimmune disorders such as Lupus, Rheumatoid arthritis, etc. The immune system just finds a different target.
We need to rebalance the immune system to prevent this. Sometimes the autoimmunity can be reversed as well! The gut determines your immune system. With the exception of discussing proper thyroid medication dosing, the majority of my website and my book focuses on balancing the immune system. The info I present is based on my own research and journey for overcoming my autoimmune thyroid condition. Here are a couple articles you might find interesting:
IMPORTANCE OF GUT HEALTH
https://bruno-michael-wentz.dev01.rmkr.net/articles/importance-gut-health/
WHERE DO I START WITH HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/where-do-i-start-with-hashimotos/
HASHIMOTO’S AND GRAVES’ REMISSION AFTER HELICOBACTER PYLORI ERADICATION
http://bruno-michael-wentz.dev01.rmkr.net/articles/hashimotos-and-graves-remission-after-helicobacter-pylori-eradication/