Hydration may not be the first thing you think of when it comes to Hashimoto’s and thyroid health, but having adequate levels of water is absolutely essential for all areas of health — and electrolytes play a crucial role in ensuring we stay hydrated.
People with certain health concerns — including thyroid conditions and adrenal imbalances — may be more prone to dehydration caused by electrolyte imbalance, and may be more intensely affected by symptoms. [1]
Throughout my Hashimoto’s journey, I’ve felt the effects of low electrolytes. It was probably not a coincidence that these symptoms of headaches, feeling dizzy when I stood up, and fatigue, correlated with my autoimmune flares… and seemed to resolve again when I was able to address their root cause.
While I make it a point to regularly consume high-electrolyte foods such as sea salt and bone broth, I often turn to supplements for extra support — especially after intense exercise, and during periods of higher stress.
Staying hydrated and replenishing our electrolyte levels is an important part of healing, and can help reduce symptoms that may often be attributed to “just having a thyroid condition,” including fatigue, constipation, dry skin, and many others.
In this article, you will learn:
- Symptoms and causes of electrolyte imbalances
- The electrolyte-Hashimoto’s connection
- The role of the adrenals
- How to know if you need electrolytes
- Food sources and supplements to replenish your electrolyte levels
What Are Electrolytes?
Electrolytes are minerals that play a critical role in the body. Through a biochemical process, electrolytes become ions (an atom or molecule with an electrical charge) that can conduct electrical signals in the body. These signals create communication and function within nerves and muscles, as the electrolytes move in or out of cells. Electrolytes are important for fluid balance, muscle contraction, and blood pressure, and play other roles in the body as well.
Electrolytes include:
- Sodium
- Potassium
- Calcium
- Magnesium
- Chloride
- Phosphate
- Bicarbonate
Potassium is the main intracellular (inside the cell) ion, and sodium is the main extracellular (outside the cell) one. Potassium and sodium get the most attention for this reason, and are arguably the most important for maintaining good hydration and electrolyte balance within the body. Sodium and potassium function in the body in a very specific balance.
The pituitary gland in the brain helps to manage electrolytes throughout the body. It can be hard to measure true electrolyte status because at times, the body needs to prioritize where electrolytes go. So, it is possible for one’s electrolytes to appear low in one area because they are being used in another area of the body.
Electrolytes and fluid balance play a critical role in cardiovascular health, especially with heartbeat and blood pressure regulation.
Potassium is especially important due to its role in heartbeat regulation, and low (or high) potassium can create cardiac abnormalities that can potentially be life-threatening.
Historically, electrolytes were solely obtained through food, and these minerals can be found in meat and fish, bone broths, fruits, vegetables, sea salt, sea vegetables, and teas. It wasn’t until the 1920s or 30s that people started consuming supplemental electrolytes, mainly in a medical setting. The famous sports drink Gatorade has been around since 1967.
Today, electrolyte supplements are quite commonplace — especially for supporting the hydration needs of athletes, patients with vomiting or diarrhea, as well as those with electrolyte imbalances due to specific conditions or lifestyles. [2]
Electrolyte Imbalances
An electrolyte imbalance occurs when levels of one or more electrolytes within the body become too high or too low.
An electrolyte imbalance can be caused by: [3]
- Vomiting and/or diarrhea
- Medications such as diuretics
- Laxatives
- Dehydration from excess sweating, such as from exercise, sauna usage, or living in a hot or dry climate
- Low intake of key electrolyte minerals (low consumption of fruits and vegetables, for example)
- Eating disorders
- Diseases that impact the kidneys (eg: diabetes, kidney disease)
- Thyroid diseases such as Hashimoto’s
- An increased need for electrolytes due to a low-carb or ketogenic diet
- Too little or too much water intake
- Nutrient deficiencies
- Adrenal issues (including HPA-axis dysfunction/adrenal dysfunction)
- Pregnancy
Hyponatremia (low sodium in the blood) is a common form of electrolyte imbalance for those with hypothyroidism. It tends to be more common in older adults, those with hypertension (high blood pressure), heart disease, adrenal issues, and kidney disease. Symptoms include headaches, nausea, vomiting, muscle cramps, fatigue, and fainting. In extreme cases, hyponatremia can cause disorientation, seizures, brain damage, and coma. [4]
Hypernatremia (high sodium in the blood) is much less common than hyponatremia for those with Hashimoto’s. Symptoms may include weakness, nausea, loss of appetite, muscle twitching, and more severely, mental confusion, and bleeding in the brain. [5]
Hypokalemia (low potassium in the blood) is another electrolyte imbalance and may present as fatigue, constipation, frequent urination, muscle weakness, and most severely, muscular paralysis and abnormal heart rhythms. Hyperkalemia (high potassium in the blood) is also associated with abnormal heart rhythms, a slowed heart rate, and weakness. [6]
If you’re experiencing any of the symptoms listed above, you may want to monitor your electrolyte levels to see if they may be related to severe electrolyte imbalances. (I’ll address how to check your electrolyte levels further on in this article.)
But what if your levels appear to be within a “normal” range? As with all things in Hashimoto’s, I’m always looking at optimizing our levels, and want to highlight that there is still the possibility that you may have subclinical or subtle electrolyte imbalances.
In other words, it is possible to have low electrolytes, or an imbalance of electrolytes, that is less severe, but that can still affect your health (especially thyroid health and adrenal health) and contribute to symptoms. (For example, some of my clients have tested their sodium and potassium levels and were told that their levels were within normal range, yet they benefited from balancing their electrolyte levels.)
Addressing subclinical electrolyte imbalances is especially important if you’re experiencing fatigue.
The Electrolyte-Hashimoto’s Connection
Symptoms of both hyponatremia and hyperkalemia, including fatigue, weakness, low blood pressure, and even some GI symptoms, sound a lot like symptoms of hypothyroidism — which makes sense, since the thyroid and electrolytes are intimately connected.
Research suggests that electrolyte imbalances directly correlate with thyroid imbalances. This is partly due to the fact that thyroid abnormalities may lead to changes in kidney function, which in turn can lead to electrolyte imbalances.
Plus, thyroid hormones are involved in the metabolism of minerals. As such, people with hypothyroidism, especially advanced cases of hypothyroidism, generally experience a slower metabolism, resulting in electrolyte abnormalities. However, the basic mechanisms of how thyroid hormones influence electrolytes are not fully understood. [7]
One study that aimed to find out the effect of hypothyroidism on electrolyte and mineral levels, looked at 140 cases of overt hypothyroidism from whom blood samples were collected. Their T3, T4, and TSH levels were measured. Calcium, phosphorus, magnesium, sodium, and potassium levels in the blood were also measured. The researchers concluded that the higher the TSH levels one had, the higher the magnesium and phosphorus levels were in the blood, and the lower the values of serum calcium, sodium, and potassium levels were. Thus, they found that the more severe one’s hypothyroidism is, the more severe their electrolyte imbalances may be. [8]
In yet another study, participants with hypothyroidism showed low serum sodium, chloride, and potassium levels. Conversely, those with hyperthyroidism had increased serum potassium levels. [9]
Another study conducted on 110 clinically known cases of hypothyroidism between the ages 20 and 60, demonstrated similar findings. The hypothyroid patients in their study showed serum electrolyte disturbances, such as low sodium, potassium, and calcium levels, as well as high magnesium and phosphorus levels. [10]
In most cases of electrolyte imbalance for those with hypothyroidism, the proper dose of thyroid medications should help to restore electrolyte balance. However, researchers have found that hydration status can actually complicate getting the right dose of thyroid medication by interfering with thyroid labs. In one study, TSH levels were eight percent higher in those who were dehydrated, compared to those with optimal hydration status. [11]
The good news is that this can reverse rapidly with hydration. If your TSH is a little higher than normal and you’re experiencing thyroid symptoms, part of that could be due to hydration, and increasing your water and/or electrolyte intake will increase the efficiency of your thyroid hormones.
The bottom line is that addressing thyroid hormone imbalances due to hypothyroidism, and paying attention to hydration, play an important part in addressing electrolyte imbalances and healing with Hashimoto’s.
The Role of the Adrenals
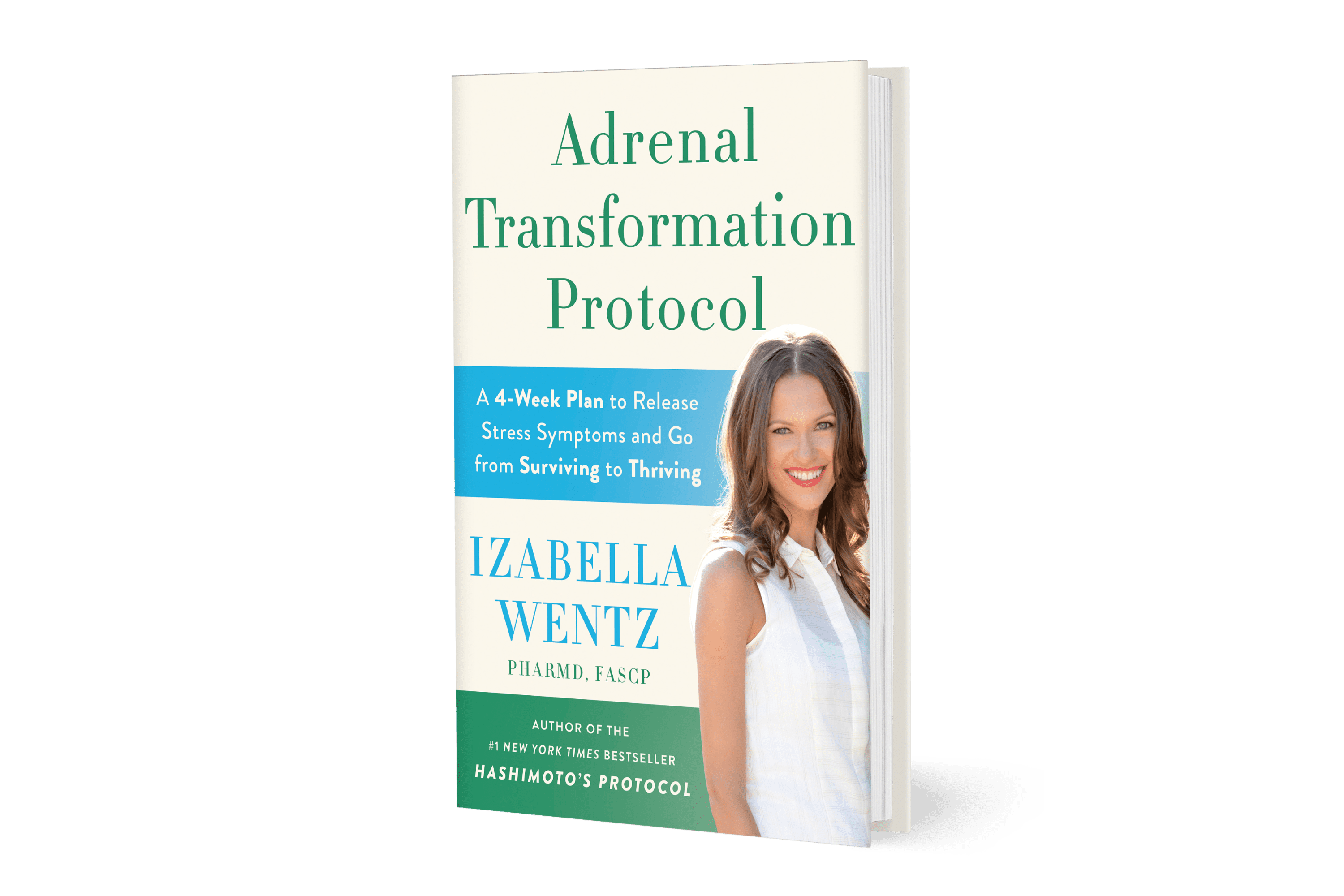
Through my clinical experience and research, I’ve learned that dehydration, nutrient deficiencies, and adrenal issues are interconnected with each other, as well as thyroid disease. Addressing adrenal imbalances can relieve some of the symptoms associated with Hashimoto’s. (Read my new book about adrenal dysfunction to learn more about how to balance your adrenals.)
Addressing thyroid health without addressing the adrenals can often further deplete the adrenals, making Hashimoto’s symptoms worse.
The adrenals (adrenal glands) are responsible for the production of many hormones which play an important role in electrolyte balance.
Aldosterone is a hormone made by the adrenal glands that helps to regulate blood volume, blood pressure, and sodium/potassium levels. When the adrenal glands are weakened (in the advanced stages of adrenal dysfunction), sodium levels become unregulated and can fall too low, causing an electrolyte imbalance. This is the mechanism behind low blood pressure that often accompanies adrenal and thyroid imbalances. [12]
The adrenal glands also make glucocorticoid hormones like cortisol. When there is too much cortisol, thyroid hormone production is typically suppressed, and the conversion of T4 to T3 may also be impaired by suppressing the 5’deiodinase enzyme. [13]
It makes sense that the body would suppress the activation of thyroid hormone under conditions of stress. I believe that this is one of the body’s innate protective mechanisms used to conserve nutrients and resources so that they can be used to promote healing instead. (I have developed my own theory, which I call the Safety Theory, about the development of autoimmune thyroid disease — you can read more about that here.)
The problem today, however, is that in our modern world, we face different and constant stressors (toxins, negative thoughts, balancing work and family, sitting in traffic, etc.) — and these signals can promote some of the unwanted symptoms of Hashimoto’s, including weight gain, depression, and fatigue. [14]
Chronic stress is all too common in our society and can lead to adrenal dysfunction. Besides the sodium imbalance discussed here, constantly high levels of cortisol can deplete both potassium and magnesium (along with zinc, iron, copper, vitamin C, and B vitamins). [15] If you feel dizzy upon standing, are prone to fainting, feel thirsty, and crave salty foods, these symptoms may be linked to adrenal dysfunction.
Taking a deeper look at the adrenals (and electrolytes!) is an important root cause approach to healing.
Years ago, when I was searching for remission from Hashimoto’s, I had never heard of adrenal dysfunction — I wasn’t even sure it was a real condition (many conventional doctors do not consider it to be “real”). Not only did my compounding pharmacist assure me that adrenal dysfunction was real, but also helped me realize that I had it. When I started to use protocols to address this, I noticed some amazing improvements: I felt more focused, my energy levels improved, and my fatigue dissipated.
Years later, when I became a new mom and found myself in adrenal dysfunction once more, I was able to find an approach to healing, even though my lifestyle wasn’t (and still isn’t) perfect.
I knew that my body was responding to the various stress symptoms in the environment, and I decided to send it safety signals instead, to put it into a healing and rebuilding state.
The protocol worked so well for me, I decided to pilot it as a program with a small group in 2020! Despite all of the things that had happened in 2020, people reported that the program helped them re-balance their stress response. Results from this Adrenal Transformation Program were amazing — 89 percent reported reduced fatigue, 86 percent reported reduced anxiety, and 81 percent respectively reported improved sleep (these are just a few of many positive outcomes). I was so excited with these results that I decided to write a book, Adrenal Transformation Protocol, which details a simple four-week plan designed to help you recover your energy and get back to your normal self again!
So if you think you might have adrenal dysfunction, rest assured that it is possible to recover, and two important aspects of healing are restoring nutrient balance and maintaining good hydration. This is all tied in with improving thyroid health as well!
(I also cover adrenal protocols in my 2017 book, Hashimoto’s Protocol — but since I got so much feedback about adrenals specifically, the protocols in my new book are much more evolved and advanced. :-))
When I surveyed my Hashimoto’s readers, some 90 percent reported some level of adrenal dysfunction! In testing clients, the majority of them presented with some adrenal dysfunction, and most notably, the most common pattern was low cortisol.
How Can I Tell If My Electrolyte Levels Are Low?
Electrolytes are often measured as part of routine annual lab work with your primary care provider, but you can certainly request these labs more often. If your blood levels of sodium, potassium, or calcium are out of the normal lab range, this would signal a severe electrolyte imbalance. This is the main way that conventional medicine looks at electrolytes. [16]
That said, as mentioned earlier, some cases of electrolyte imbalances may be “subclinical.” In other words, it is possible to have low levels of certain electrolytes, or an imbalance of electrolytes that is less severe, but still affects your thyroid health.
After all, the body, which needs pretty tight control of electrolytes in the blood, may prioritize electrolytes and concentrate them in certain areas when there is a deficiency somewhere.
Symptoms of electrolyte imbalance, Hashimoto’s, and adrenal imbalance can all overlap to some degree.
Here are some common symptoms to look for:
- Fatigue (even after a good night’s sleep)
- Salt cravings
- Low blood pressure
- Feeling faint from standing
- Brain fog
- Low blood sugar
- Hitting the snooze button
- Feeling “wired, but tired”
- Mild depression
- Decreased resilience to stress
- Headaches
- Muscle aches or cramps
- Diarrhea or constipation
- Frequent urination (including drinking water and feeling the urge to urinate right away)
- Fast or irregular heartbeat
- Increased thirst
- Anxiety
- Dry skin and lips
If you experience a collection of these symptoms, you may experiment with increasing electrolytes to see if that helps to improve your symptoms. (I’ll discuss ways to increase your levels below!)
Please note that electrolyte imbalances may be compounded by intense exercise, living in a hot or dry climate, and drinking caffeine or alcohol. If any of these are true for you, you may need more water and electrolytes than you think.
Food Sources of Electrolytes
Electrolyte levels can be replenished through food and beverages, over-the-counter supplementation, or via an IV drip for more serious cases.
It is generally very safe to consume electrolytes from food, and it is truly a foundational approach to addressing electrolyte imbalance. I have found that most people with Hashimoto’s need more sodium, potassium, and magnesium, but it’s important to note that there may be some cases where this doesn’t hold true. For example, in cases where potassium is high relative to sodium, eating high-potassium foods may make someone feel worse.
A Standard American Diet is full of highly processed foods associated with high sodium (and generally low in potassium and magnesium) intake. If you are eating a whole foods-based, anti-inflammatory diet to address Hashimoto’s — such as what I share in Hashimoto’s Food Pharmacology: Nutrition Protocols and Healing Recipes to Take Charge of Your Thyroid Health — you may actually need more salt than what you are getting from your food.
One sign that you need more sodium is having salt cravings.
My best tip is to eat more salt, but the right kind of salt! Iodized salt is partially responsible for the Hashimoto’s epidemic (read my article to find out why!), so it is important to choose non-iodized varieties. I like to use Celtic sea salt or Himalayan pink salt.
Besides liberally salting food, salted bone broth is a great option for hydration. In the 2015 survey I conducted on people with Hashimoto’s, participants reported that homemade broth helped with energy, mood, weight, pain, hair, skin, and thyroid labs!
To increase electrolytes through food, here are some of the best sources of sodium, potassium, and magnesium (which many people with Hashimoto’s are also deficient in).
Most of the foods listed here are safe and appropriate for the type of food plan that I often recommend to my clients, in the interest of reducing Hashimoto’s symptoms (check out this article on the best diet for Hashimoto’s for more information). Please also use caution with known or suspected food sensitivities.
High-Sodium Foods
- Sea salt (be sure to choose non-iodized varieties)
- Bone broth
- Celery
- Pickles, sauerkraut, and other fermented foods
- Seafood
High-Potassium Foods
- Bananas
- Sweet potatoes
- Potatoes
- Coconut water
- Avocados
- Winter squash
- Beans
- Dried apricots
- Prunes
- Raisins
- Yogurt
- Spinach
- Artichoke
- Beet greens
High-Magnesium Foods
- Kale, spinach, and other dark leafy greens
- Almonds, cashews, Brazil nuts, and other nuts
- Avocados
- Dark chocolate
- Black beans, and other beans
- Pumpkin, flax, and chia seeds
How Much Water Should I Drink?
It is important to also focus on drinking enough water as you work on balancing your electrolytes. You may need eight to ten glasses per day, and more with exercise or caffeinated beverages.
To determine the precise amount of water your body needs, here is a simple calculation to work with:
Calculate half your body weight in pounds, then aim to drink that number of ounces of water per day. For example, a 150-pound person would aim to drink 75 ounces of water per day.
You may need to help keep yourself on track with water intake. I recommend either writing a daily water goal in your journal, or drawing the number of glasses you need, and filling them in daily. You can also use a free water counting app on your smartphone (like Waterlogged) to track your daily water intake.
If you’re at home, my personal favorite is to make a pitcher of spa water each morning (by adding cut-up cucumbers, strawberries, lemons, and/or limes to a pitcher of purified water), and sipping on it throughout the day.

However, while it’s unlikely that most people will do so, I do want to mention that it’s possible to drink too much water. Water intake can contribute to electrolyte imbalance. Feeling weak, having headaches, and experiencing vomiting and nausea, are the most common signs of water over-consumption. Symptomatic water intoxication has been observed when a person drinks about three to four liters (.75 – 1 gallon) of water at one time, but this can be avoided by spacing your water consumption out throughout the course of the day. [17]
Electrolyte Drinks and Supplements
A great way to replete electrolytes in a relatively short time is by using electrolyte supplements. A word of caution, however, is that a lot of electrolyte products, including sports drinks such as Gatorade, are not necessarily healthy options because of their high levels of sugar, dyes, and flavorings. However, a little bit of natural sugar in an electrolyte supplement is okay, since glucose helps the body to absorb the electrolyte minerals.
You can make your own electrolyte drinks, and depending on if you need more or less potassium, I recommend two hydration blends that are easily made at home.
Potassium
Potassium is important for keeping fluids balanced in the body, lowering blood pressure, and addressing water retention — which in turn can help regulate the internal stress response.
How do you know if you need more or less potassium?
As mentioned earlier, you may need more potassium if you experience:
- Excessive thirst
- Salt cravings
- Water retention
- Cognitive issues
- High blood pressure
- Heartbeat fluctuations
- Nervousness
You may need less potassium if you:
- Have low blood pressure
- Are on a potassium chloride supplement
- Experience GI symptoms such as nausea or vomiting
If you are experiencing any of these symptoms, I recommend that you consult with your practitioner to test your potassium levels via a blood test, to see if either of these hydration blends are optimal for you.
More Potassium Blend:
- 1 quart of coconut water
- ¼ – ½ teaspoon sea salt (gray or pink)
Less Potassium Blend:
- 1 quart filtered water
- ½ teaspoon sea salt (gray or pink)
Sodium
Sodium has gotten a bad rap in the medical industry. However, it is crucial for regulating fluids in the body. As mentioned above, I recommend using sea salt or Himalayan pink salt, as opposed to table salt or iodized salt.
Salt nourishes the adrenals and provides the minerals, such as potassium and magnesium, that our body needs. It also offers us hydration when we are in a dehydrated state, by keeping fluid in the body (also known as water retention).
How do you know if you need more sodium?
You will want to see if you have:
- Salt cravings
- Excessive thirst that is not alleviated by drinking plain water
- Excessive fluid loss, such as sweating or urinating
- Recently engaged in high-intensity exercise
- Diluted urine
How do you know if you need less sodium?
You may be:
- Someone with high blood pressure
- A sodium-sensitive individual (blood pressure rises with sodium, and lowers when omitting sodium)
- A salt-resistant individual (blood pressure doesn’t change with sodium dose change)
Here’s a recipe for “Sole,” a high-concentration mixture of Himalayan sea salt and filtered water. This salt mixture can be taken once per day, up to 1 teaspoon at a time, on an empty stomach.
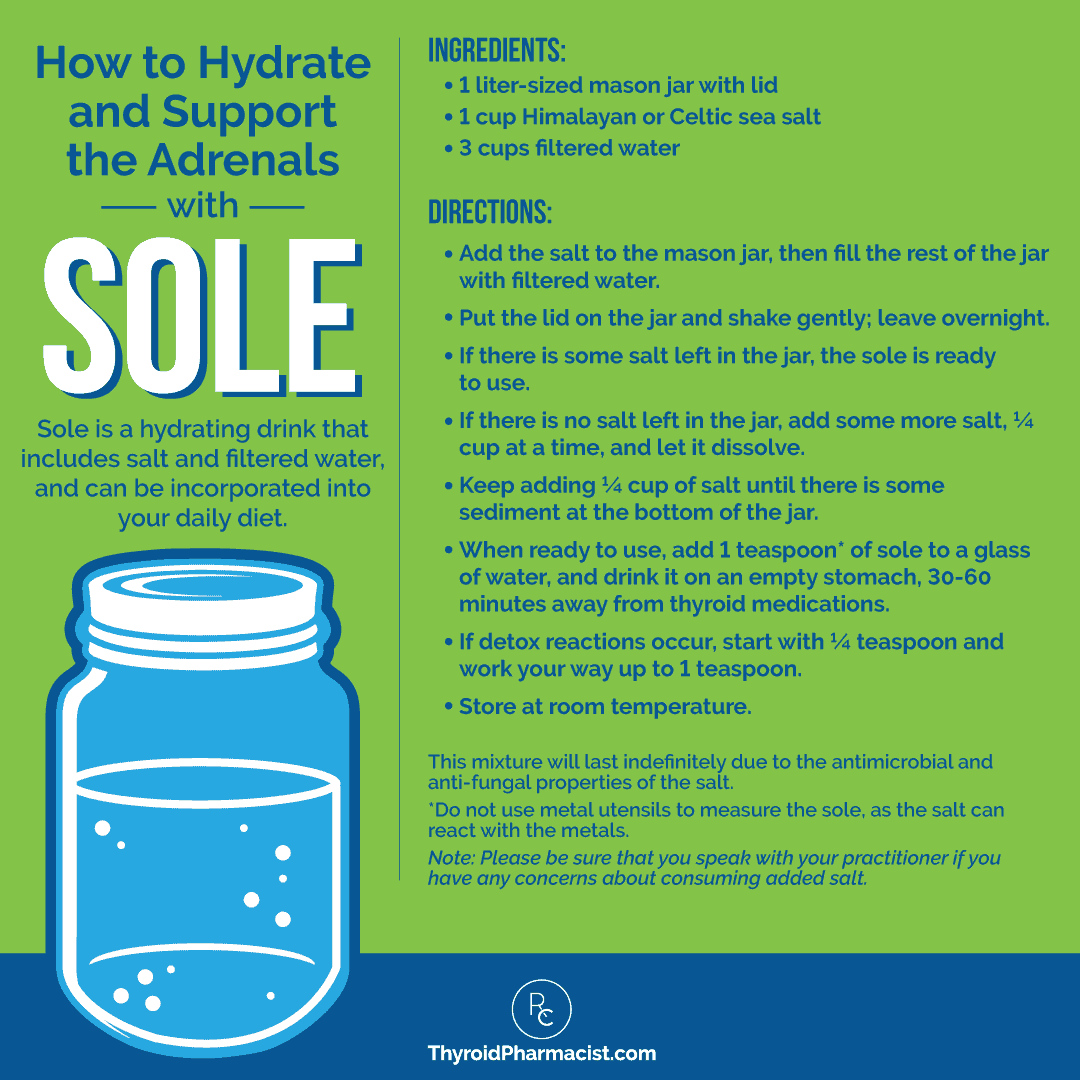
You can make your own, or if you want to keep it super simple, you can purchase this Sole kit from Symphony Natural Health.
Supplement Options
You can also supplement with an electrolyte blend.
I developed Rootcology Electrolyte Blend as a complete and balanced formula, specifically to support people with Hashimoto’s. This formula contains the electrolytes sodium, potassium, chloride, and magnesium, along with additional thyroid-supporting ingredients, including:
- Vitamin C – An important antioxidant to support the adrenals, mitochondria, thyroid hormone, and collagen production. Researchers are also finding that vitamin C may have antiviral properties and may be helpful in recovering from viral infections, such as the Epstein-Barr virus. [18]
- D-ribose – A natural sugar that supports mitochondrial health, energy production, and exercise recovery. Research suggests that D-ribose can help provide more energy in chronic fatigue syndrome. [19]
- Bioflavonoids – Quercetin and citrus bioflavonoids work synergistically with vitamin C to reduce inflammation. They also have antihistamine and antiviral properties. [20]
- Taurine – An amino acid that supports the gallbladder (according to my estimates, about 30-50 percent of people with Hashimoto’s may have gallbladder issues), helps remove fluoride from the body, aids digestion, helps with allergies, and supports healthy blood pressure through electrolyte regulation in the cells. [21]
This blend may be helpful for supporting cardiovascular health, blood pressure, and fluid balance, recovering from a cold or flu, replenishing electrolytes during and after sweating, supporting the adrenals, and mitigating symptoms of dehydration. (I usually recommend 1 teaspoon of Rootcology Electrolyte Blend in eight to ten ounces of water each day, or as directed by your personal provider. As always, please consult with your practitioner to ensure this supplement is right for your needs.)

Here’s what Kate had to say:
“I follow you on Facebook and read one of your articles about the Electrolyte Blend. I thought, what have a got to lose? My chiropractor was always telling me ‘you’re dehydrated’..and I was like HOW I drink a ton of water. Well apparently I was, I don’t know! Lol. The Electrolyte Blend gave me calm. No more heart palps and TMI, but I am ‘regular’ for the first time in my life! Adding the electrolyte blend is the only change I have made. I have more energy but it doesn’t like crazy energy for Hashi’s! I would think this is a huge help to my busted adrenals as well since I feel calm 🙂 Thank you!”
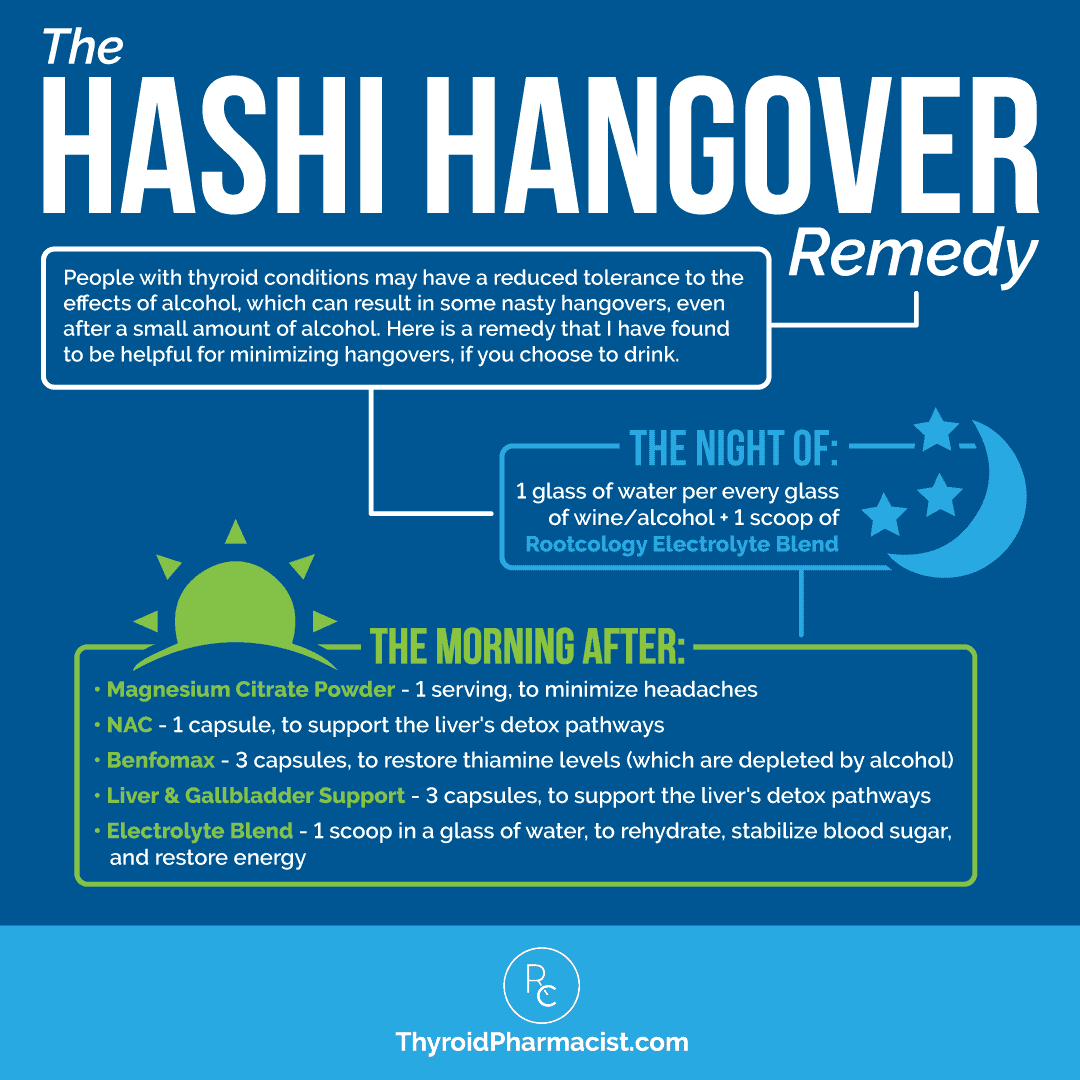
It is also useful to have on hand when enjoying an occasional glass of wine, or two. 🙂 When drinking alcohol, have 1 scoop in a glass of water along with each drink. (Do not exceed more than 1 scoop of Rootcology Electrolyte Blend per day.) You may want to have an additional scoop the next morning as well! This is very helpful for preventing the symptoms of a hangover, by keeping you hydrated.
You can also mix Rootcology Electrolyte Blend into smoothies, or use the blend to make popsicles, which are great for a hot day or when you’re down with the flu. I also like to have a scoop after a yoga class or hike, especially if I worked up a sweat.
Warnings/Precautions
Electrolyte supplements may not be recommended for those with sodium-sensitive hypertension, those with a pacemaker, and those with high sodium or potassium levels. Do not use if you are allergic or sensitive to any of the ingredients in this supplement.
Consult with a doctor before use if pregnant or breastfeeding.
Do not take if taking the following medications: ACE inhibitors, aminoglycoside antibiotics, anticoagulant/antiplatelet drugs, antihypertensive drugs, antidiabetic drugs, angiotensin receptor blockers, antacids, bisphosphonates, blood thinners, calcium channel blockers, corticosteroids, didanosine, digoxin, insulin, levodopa/carbidopa, lithium, potassium-sparing diuretics, quinolone antibiotics, skeletal muscle relaxants, sodium phosphates, sulfonylureas, tetracycline antibiotics, or tolvaptan.
Please note: Electrolyte Blend contains ingredients derived from non-GMO corn, but does not contain the corn protein component which can cause allergies. While it is generally well-tolerated by those with corn sensitivities, please consult with your practitioner before use if you have individual concerns.
Next Steps
While balancing electrolytes isn’t a cure for Hashimoto’s, it can be one piece of your root cause puzzle, since everything in the body is interconnected. Dehydration and an increased need for electrolytes are quite common with thyroid issues, especially since adrenal issues are typically also involved, and there is a studied correlation between thyroid hormone and electrolyte levels.
Electrolytes may be helpful in reversing some of the symptoms of dehydration that overlap with symptoms of Hashimoto’s or adrenal dysfunction — and, for some, electrolytes may even help to improve thyroid labs. The electrolyte minerals, specifically sodium, potassium, and magnesium, are generally very nourishing for the thyroid!
I always believe in a food-first and food-as-medicine approach. In this case, including a lot of mineral-rich whole foods, non-iodized sea salt, and bone broths is foundational. Since electrolyte supplements, like Rootcology Electrolyte Blend, are safe for most people and are also an effective way to address dehydration, that may be another area to experiment with, to provide the body with some support.
If you are struggling with fatigue and other symptoms that may indicate adrenal dysfunction, I highly encourage you to investigate your adrenal health, and consider my newest book, Adrenal Transformation Protocol. The book is designed to help you identify your adrenal triggers, balance your stress response, and build up your resilience to prevent excess stress from overwhelming your adrenals again.
Supporting the adrenals can result in profound improvements in energy levels, help you feel more calm, and allow the body to repair itself in just a few weeks, so that you feel like yourself again!
Now I want to hear from you! How have you used electrolytes in your healing journey?
P.S. I love staying in touch with my readers! To stay on top of thyroid health updates and meet others who are following similar health journeys, please join my Facebook, Instagram, TikTok, and Pinterest community pages. For recipes, a Thyroid Diet start guide, notifications about upcoming events, and the Nutrient Depletions and Digestion chapter from my first book for free, be sure to sign up for my email list!
References
[1] Liamis G, Filippatos TD, Liontos A, Elisaf MS. MANAGEMENT OF ENDOCRINE DISEASE: Hypothyroidism-associated hyponatremia: mechanisms, implications and treatment. Eur J Endocrinol. 2017;176(1):R15-R20. doi:10.1530/EJE-16-0493; All About Electrolyte Disorders. Healthline. Updated April 29, 2019. Accessed May 4, 2022. https://www.healthline.com/health/electrolyte-disorders
[2] West H. Electrolytes: Definition, Functions, Imbalance and Sources. Healthline. Updated October 24, 2018. Accessed May 4, 2022. https://www.healthline.com/nutrition/electrolytes; Electrolytes. Cleveland Clinic. Updated September 24, 2021. Accessed May 4, 2022. https://my.clevelandclinic.org/health/diagnostics/21790-electrolytes; How too little potassium may contribute to cardiovascular disease. National Institutes of Health. October 24, 2017. Accessed June 5, 2022. https://www.nih.gov/news-events/nih-research-matters/how-too-little-potassium-may-contribute-cardiovascular-disease
[3] Mount, David B. Hyponatremia and hyperkalemia in adrenal insufficiency. UpToDate. 2022. Wolters Kluwer. Accessed June 5, 2022. https://www.uptodate.com/contents/hyponatremia-and-hyperkalemia-in-adrenal-insufficiency; Electrolyte imbalance symptoms, what causes it, and how to treat it. Medical News Today. Healthline Media, 2022. Accessed June 5, 2022. https://www.medicalnewstoday.com/articles/electrolyte-imbalance; Alqahtani HA, Almagsoodi AA, Alshamrani ND, Almalki TJ, Sumaili AM. Common Electrolyte and Metabolic Abnormalities Among Thyroid Patients. Cureus. 2021;13(5):e15338. Published 2021 May 30. doi:10.7759/cureus.15338
[4] Lawless SJ, Thompson C, Garrahy A. The management of acute and chronic hyponatraemia. Ther Adv Endocrinol Metab. 2022;13:20420188221097343. Published 2022 May 14. doi:10.1177/20420188221097343; Liamis G, Filippatos TD, Liontos A, Elisaf MS. MANAGEMENT OF ENDOCRINE DISEASE: Hypothyroidism-associated hyponatremia: mechanisms, implications and treatment. Eur J Endocrinol. 2017;176(1):R15-R20. doi:10.1530/EJE-16-0493
[5] Reynolds RM, Padfield PL, Seckl JR. Disorders of sodium balance. BMJ. 2006;332(7543):702-705. doi:10.1136/bmj.332.7543.702
[6] Viera AJ, Wouk N. Potassium Disorders: Hypokalemia and Hyperkalemia. Am Fam Physician. 2015;92(6):487-495.
[7] Schwarz C, Leichtle AB, Arampatzis S, Fiedler GM, Zimmermann H, Exadaktylos AK, Lindner G. Thyroid function and serum electrolytes: does an association really exist? Swiss Med Wkly. 2012;142:w13669. Doi: 10.4414/smw.2012.13669; Kaur J, Ahmad N, Gupta A. Changes in the Electrolyte Profile of Patients having Hypothyroidism. Journal of Medical Science and Clinical Research. ISSN (e)-2347-176x Volume 2. Issue 4. Page 633-637. April 2014.
[8] Murgod R, Soans G. Changes in Electrolyte and Lipid Profile in Hypothyroidism. International Journal of Life Sciences & Pharma Research. ISSN 2250-0480 Vol Issue 3. Jul-Sept 2012.
[9] Abebe N, Kebede T, Wolde M. Assessment of renal function and electrolytes in patients with thyroid dysfunction in Addis Ababa, Ethiopia: a cross sectional study. Pan Afr Med J. 2016;24:338. Published 2016 Aug 31. doi:10.11604/pamj.2016.24.338.8455
[10] Kaur J, Ahmad N, Gupta A. Changes in the Electrolyte Profile of Patients having Hypothyroidism. Journal of Medical Science and Clinical Research. ISSN (e)-2347-176x Volume 2. Issue 4. Page 633-637. April 2014.
[11] Ybarra J, Fernandez S. Rapid and reversible alterations in thyroid function tests in dehydrated patients. Nurs Clin North Am. 2007;42(1):127-34.
[12] Mount, David B. Hyponatremia and hyperkalemia in adrenal insufficiency. UpToDate. 2022. Wolters Kluwer. Accessed June 5, 2022. https://www.uptodate.com/contents/hyponatremia-and-hyperkalemia-in-adrenal-insufficiency
[13] Hidal JT, Kaplan MM. Inhibition of thyroxine 5′-deiodination type II in cultured human placental cells by cortisol, insulin, 3′, 5′-cyclic adenosine monophosphate, and butyrate. Metabolism. 1988;37(7):664-668. doi:10.1016/0026-0495(88)90087-x
[14] Ranabir S, Reetu K. Stress and hormones. Indian J Endocrinol Metab. 2011;15(1):18-22. doi:10.4103/2230-8210.77573
[15] Lopresti AL. The Effects of Psychological and Environmental Stress on Micronutrient Concentrations in the Body: A Review of the Evidence. Adv Nutr. 2020;11(1):103-112. doi:10.1093/advances/nmz082
[16] Electrolytes. Cleveland Clinic. Updated September 24, 2021. Accessed May 4, 2022. https://my.clevelandclinic.org/health/diagnostics/21790-electrolytes
[17] What happens if you drink too much water? Medical News Today. Healthline Media, 2022. Accessed June 5, 2022. https://www.medicalnewstoday.com/articles/318619
[18] Mikirova N, Hunninghake R. Effect of high dose vitamin C on Epstein-Barr viral infection. Med Sci Monit. 2014;20:725-732. Published 2014 May 3. doi:10.12659/MSM.890423
[19] Teitelbaum JE, Johnson C, St Cyr J. The use of D-ribose in chronic fatigue syndrome and fibromyalgia: a pilot study. J Altern Complement Med. 2006;12(9):857-862. doi:10.1089/acm.2006.12.857; Jones K, Probst Y. Role of dietary modification in alleviating chronic fatigue syndrome symptoms: a systematic review. Aust N Z J Public Health. 2017;41(4):338-344. doi:10.1111/1753-6405.12670
[20] Park HH, Lee S, Son HY, et al. Flavonoids inhibit histamine release and expression of proinflammatory cytokines in mast cells. Arch Pharm Res. 2008;31(10):1303-1311. doi:10.1007/s12272-001-2110-5; Anand David AV, Arulmoli R, Parasuraman S. Overviews of Biological Importance of Quercetin: A Bioactive Flavonoid. Pharmacogn Rev. 2016;10(20):84-89. doi:10.4103/0973-7847.194044
[21] Yang JY, Zhang TT, Yu ZL, et al. Taurine Alleviates Trimethylamine N-Oxide-Induced Atherosclerosis by Regulating Bile Acid Metabolism in ApoE-/- Mice. J Agric Food Chem. 2022;70(18):5738-5747. doi:10.1021/acs.jafc.2c01376; Adedara IA, Olabiyi BF, Ojuade TD, Idris UF, Onibiyo EM, Farombi EO. Taurine reverses sodium fluoride-mediated increase in inflammation, caspase-3 activity, and oxidative damage along the brain-pituitary-gonadal axis in male rats. Can J Physiol Pharmacol. 2017;95(9):1019-1029. doi:10.1139/cjpp-2016-0641; Nam SY, Kim HM, Jeong HJ. The potential protective role of taurine against experimental allergic inflammation. Life Sci. 2017;184:18-24. doi:10.1016/j.lfs.2017.07.007.
Note: Originally published in April of 2020, this article has been revised and updated for thoroughness and accuracy.


 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
I leaned a lot from this article, but I have a question about potassium. The article mentions that potassium helps lower blood pressure, but then says someone may need more potassium if they have low blood pressure and conversely may need less potassium if they have high blood pressure. Wouldn’t it be the opposite of potassium lowers blood pressure?
Regina – Thank you so much for pointing this out to me. You were right, it was confusing! To better explain, potassium does help lower blood pressure by balancing out high sodium levels, so someone may need less potassium if they have low blood pressure; and conversely, they may need more potassium if they have high blood pressure. I hope that helps! <3
THANK YOU SO MUCH! This article is right on target for me. I experienced SEVERE heart palps, off & on, for 1.5 yr. I kept asking my Dr. if it was time to decrease my thyroid dose. Finally, last straw was in December 2019, Heart rate & BP were out the roof. GOT home from work & called Dr., demanding we do something. Took me off dessicated thyroid T3/T4, put on Levothyroxine T4 only. 2 weeks later more heart palps. Called compounding pharmacist & Dr. and back on compounded T4 only. However, I did speak to a customer, at my work (she was buying bananas) who had just been hospitalized (by ER visit) for the same symptoms as myself & she told me about electrolytes. She refused to leave the hospital until they ran ALL tests to get to the bottom because she had experienced the same for quite a while. Also warned against beta blockers, which she refused & my Dr had thoughts of at one point. After talking to her, I started drinking the bottled purified water w/electrolytes.
My Dr. is a Natural Health DO. Needless to say I am losing faith because it should not have taken 1.5 yr to get things figured out, which adjusting the thyroid med, I know now, was not the complete answer. Now I may not be getting T3/T4 balance, without T3.
I have to do compounded scripts because with Hashimotos I am also Celiac w/ corn allergy. So, thank you, Dr. Wentz! I intend to print this and present it at my next appointment. I get labs in July & office visit in August.
Dawn – thank you so much for sharing your journey with me! <3 I'm so proud of your for taking charge of your health and I hope you will keep me posted on your progress.
Thank you for this enlightening article. The body certainly is a complex thing and we are all different..so I will be ‘dabbling’ with your recommendations and see what differences I can make! Little by little.
Greetings from Australia.
Linda
LindaB – you are very welcome! <3 I hope you will keep me posted on your progress.
Could you make a supplement without stevia? I have the genetic snip that makes stevia taste bitter and nasty. In fact, my siblings and son have the same reaction to stevia.
Wendy – thank you for reaching out and sharing your feedback. <3 I'm happy to share and discuss this with my team!
Hello
I’m from Australia n would like to purchase the electrolyte. Do you post out to Australia
Teresia – thank you so much for your interest in my Rootcology products! <3 Unfortunately, we cannot currently sell or ship our Rootcology supplements outside of the United States due to complicated regulations. However, I do have an alternate recommendations for my international customers, please email my team at info@rootcology.com and they will be happy to share with you!
Thank you for your article about electrolytes affecting symptoms of Hashimoto’s. Will your Rootcology Electrolyte Blend balance out all the electrolytes even when I consume foods to obtain certain electrolytes even when some are too high or too low or just right?
Shirley – thank you for reaching out. <3 Rootcology Electrolyte Blend is a complete and balanced electrolyte formula to help promote optimal hydration, especially after excessive sweating. It contains potassium, sodium, chloride and magnesium, the main electrolytes found in the body. For any other questions about the supplement please email my team at info@rootcology.com and they will be happy to help.
Hello Dr Wentz,
I have Hashimoto’s disease and was also diagnosed with having stage 2 adrenal fatigue. I have suffered with frequent urination for 8 years now mainly due to a large fibroid resting on my bladder. But I think the frequent urination goes beyond that. Some nights are so bad that as soon as I lay down I have to go again and again…that I just may as well try and sleep on the toilet. It’s terrible and the doctors will not look beyond the fibroid. I noticed it’s worse when I’m anxious or am having stress. I did end up in the hospital in the beginning of the year with irregular heartbeat and sky high blood pressure from a lot of stress in my life. They also found that I was very dehydrated. I did feel much better after they gave me the Iv for hydration. So my question is if I keep my electrolytes up like say with your product…could that possibly help with my frequent urination? If so how much would you suggest for Someone like me with Hashimoto’s, stage 2 adrenal fatigue and I’m also Postmenopausal. I do have excessive thirst at night as well from it. My blood sugar I guess the doctors say is fine. I am so tired of this frequent urination with no help…all the doctors do is keep telling me I need surgery. 🙁 The fibroid did shrink but grew back after I stopped taking natural progesterone cream for a year. So back on that again. I’m so very frustrated and exhausted. 🙁 I would love to try your product for my electrolyte balance. BTW I hardly ever have any color to my urine even when I was dehydrated.
Tammy – thank you so much for reaching out and sharing your journey. <3 I'm so sorry you are struggling with all of this. I highly recommend that you work with a functional medicine clinician to be a part of your own health care team. It’s an entire medical specialty dedicated to finding and treating underlying root causes and prevent serious chronic disease rather than treating individual disease symptoms. I believe that everyone needs to find a practitioner that will let him/her be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It's a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://bruno-michael-wentz.dev01.rmkr.net/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://bruno-michael-wentz.dev01.rmkr.net/database-recommended-compounding-pharmacies/
Have all the above .on Armour Thyroid. All testing show my thyroid s are.balance.I also have Hashimoto’s .No insurance have to go to Health Department for labs Out of work due to the Covid19 .Anxiety out the roof . So no iodine salt . What type of diet for Hashimoto’s is best.
Karen, thank you for reaching out. <3 I always recommend starting with a diet that is gluten, dairy, corn and soy free. Here are some resources you might find helpful.
COMMON QUESTIONS ABOUT DIET AND THYROID
https://bruno-michael-wentz.dev01.rmkr.net/articles/common-questions-about-diet-and-thyroid
BEST DIET FOR HASHIMOTO’S HYPOTHYROIDISM
https://bruno-michael-wentz.dev01.rmkr.net/articles/best-diet-for-hashimotos-hypothyroidism/
DAIRY AND HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/got-hashimotos-you-may-want-to-reconsider-dairy
FOOD SENSITIVITIES AND HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/food-sensitivities-and-hashimotos
Can you advise on the best place to start? I was diagnosed with hypothyroidism in 2007. I found you 3 years ago, read Hashimotos Protocol and spent a lot of money purchasing supplements. I did that for a while and quit. It is all so overwhelming!
I read your articles and feel like I experience some symptoms of a lot of topics you discuss. Thank you!
Allison – thank you for reaching out. <3 I understand how overwhelming this can be. I believe that most nutrients should come from the diet. This is why I always list food sources in the book and on the blog, for most of the nutrients, vitamins, minerals. and probiotics that are depleted in Hashimoto’s. However, some may require or prefer supplements. I recommend getting tested for deficiencies to determine your need for a supplement as instructed in the book and blog. I also don’t recommend starting multiple supplements all at once. I recommend starting one at a time and then adding another a week or so later once it has been confirmed that the first supplement is not causing any harm. Here are some article links which might help:
WHICH SUPPLEMENTS ACTUALLY HELP HASHIMOTO'S
https://bruno-michael-wentz.dev01.rmkr.net/articles/which-supplements-actually-help-hashimotos/
USING ENZYMES TO OVERCOME HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/using-enzymes-to-overcome-hashimotos/
THE FOUR BEST PROBIOTICS FOR HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/the-four-best-probiotics-for-hashimotos/
I do have a full supplements chapter in my books. Have you checked them out? Not everyone should be taking every supplement and any of these books will help uncover your root cause. This will help you figure out your supplementation. Here are the links
Hashimoto’s Root Cause
https://amzn.to/2XXCqcQ
Hashimoto’s Protocol
https://amzn.to/3cJ89T4
Can you please advise which electrolyte(s) may be associated with muscle pain? With Hashimotos, I have many of the common symptoms, however, muscle pain in my shins, ankles and feet has been the worst issue. I consume a lot of water each day. It has taken a year to get my levels “normal.” For one month, I was starting to feel so much better, but now pain is back. Doctor says I’m just very sensitive, and does not want to change dosage. I’m wondering if I could have an electrolyte imbalance, however, my lab work was good this past January. Very frustrated, been going on for three years. (BTW, I’m gluten, dairy, and soy free.) Thank you very much.
Kelli – thank you for reaching out. <3 Please understand, I am not able to advise on what would be appropriate for you and your specific health needs without a comprehensive health assessment. I recommend that you discuss this with a practitioner who is familiar with your family history. I also highly recommend that you work with a functional medicine clinician to be a part of your own health care team. It’s an entire medical specialty dedicated to finding and treating underlying root causes and prevent serious chronic disease rather than treating individual disease symptoms. I believe that everyone needs to find a practitioner that will let him/her be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It's a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://bruno-michael-wentz.dev01.rmkr.net/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://bruno-michael-wentz.dev01.rmkr.net/database-recommended-compounding-pharmacies/
Hi Dr Izabella Wentz,
You provide a vast amount of resources which is helpful. Thank you! I take T3 only. My instructions are to take an hour before eating or drinking (other than water). I use an ORS electrolyte formula. Since the minerals are so low in electrolyte formulas is it okay to drink my electrolytes with my water during the hour I’m allowed water only?
Thank you kindly,
Alisa
Alisa – thank you for reaching out. ❤️ I’m so glad you are finding my research helpful! Thyroid medication absorption can be impacted by many things, including food, other medications, and supplements. Thyroid medication should be taken on an empty stomach, one to two hours before eating, taking other medications, supplements or coffee to ensure appropriate absorption. Antacids such as Tums, iron, magnesium, and calcium supplements can impair the absorption of thyroid medications. Thus, you need to have at least 4 hours of time in between your thyroid medications and these agents. Please be sure to read the directions provided with the medication. I hope you find this free ebook helpful. https://bruno-michael-wentz.dev01.rmkr.net/meds-ebook/
Everyone seems to recommend bone broth but I am vegan. Is there an alternative I can use?
Jean – thank you for reaching out. ❤️ I am not aware of a vegan substitute for the gelatin in the bone broth, you could search for a Vegan recipe to make a mineral-rich plant-based broth though. I hope that helps!
Is it safe to take electrolyte solutions close to the time I take my thyroid medication? I know many supplements can interfere with the absorption of levothyroxine, but I’m not sure if an electrolyte solution “counts” as a supplement. Thank you!
Katie, thank you for reaching out. ❤️ I generally recommended taking this 1-2 hours after your medications.
I have trouble drinking bone broth. I quickly goes right through me causing very loose stools. Do you have any suggestions on how to alleviate this? I would love to be able to drink this broth that everyone raves about.
Lori – thank you for reaching out. ❤️ It’s possible you are having a histamine reaction. If you are sensitive to foods that are high in histamine, you may want to avoid bone broth while you heal, as the collagen it contains is a high histamine food. There are a few ways to limit the amount of histamines in your bone broth. You can try; reducing the simmering time to four hours; using a pressure cooker to reduce cook time to 90 minutes; omitting the apple cider vinegar if you are intolerant, or use lemon juice instead. Here are a couple articles you might find helpful:
BONE BROTH: HELP YOUR GUT TO HELP YOUR THYROID
https://bruno-michael-wentz.dev01.rmkr.net/articles/bone-broth-help-gut-help-thyroid/
HISTAMINE AND HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/histamine-and-hashimotos/
Dear Izabella, can you please advise if your electrolyte powder is also to be used for children 9 years old and up? If not – why? If yes, what would be the appropriate dosage? Thank you!
Vero – thank you for reaching out. I recommend checking with you childs practitioner to be sure it is an option for them. The dosage recommendations on my supplements are for adults. ❤️
This is an amazingly insightful article! All of your info is great and has helped me with my thyroid problems. It’s so great to come here and find answers I need for continued healing. Thank you so much!
Vanessa – My pleasure! I’m so glad to hear you are finding it helpful! Please keep me posted on your progress. ❤️
Hello,
My son and I (both diagnosed now) are interested in finding support groups for beginners to this protocol. Do you have anything like that? Or know how we can find it? We are both reading our own copies of the book now, but he is way ahead of me with his learning. It is difficult to read and figure so much out when working takes the majority of my waking energy.
Thanks for any guidance you can give to help us get this ball rolling.
Blessings to you,
VM
Vicki – thank you for reaching out! I’m so glad to hear you and your son are working together on this! It’s great to have someone for support. For more support, you could check out my FB page https://www.facebook.com/ThyroidLifestyle and connect with myself as well as others there. I also recommend searching for Hashimoto’s support groups out there as well. I have found them to be really helpful. I do offer a Liver Reset program and an Adrenal Reset program and they have FB groups offered to help support the members through those. If you would like information on those programs please email my team at info@thyroidpharmacist.com and they will be happy to help you.
Is taking electrolytes first thing in AM ok mixed in the water I am taking my levothyroxine in?
Mike – thank you for reaching out. You would want to take your electrolytes 30 to 60 minutes after you take your thyroid medications.
Is there any way to try a sample of Rootcology? I’m so broke but my health is just getting worse and worse even as my lifestyle gets healthier and healthier.
Thank you for all of this information. I can’t pinpoint what caused this but I suspect following Dr. Brownsteins advice of iodine supplementation for a couple years pretty regularly might have contributed. Pretty sad and skeptical about that possibility. I just can’t afford proper medical care. Have to experiment on myself like a guinea pig.
Jay – thank you for reaching out. Currently, we do not offer samples. We do offer a 100% satisfaction guarantee, if for any reason, you are unsatisfied with a Rootcology product, it may be returned within 30 days of purchase for a full refund, minus shipping/handling fees. I’m so sorry you had this experience with iodine. I am very hesitant in recommending iodine in Hashimoto’s. Although iodine serves as fuel for our thyroid and is very important in iodine deficiency hypothyroidism, Hashimoto’s is a different mechanism. It’s like pouring gas into an engine that’s on fire… that’s essentially what’s happening in Hashi’s, thyroid inflammation. Adding iodine to the mix before putting out the fire and fixing the engine may result in further damage to the thyroid. In those with a predisposition to autoimmunity, this has been documented time and time again, in animal and human studies.
I have spent 4 years researching about this issue, and have seen too many people suffering the consequences of adding iodine too soon. My approach is, let’s fix the engine first (usually a gut issue), and then add the fuel once we know that the engine is no longer on fire. Here is an article that you might find interesting:
IODINE AND HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/iodine-hashimotos/
Hi Dr. Wentz, thank you so much for all the work you do! It has been a lifesaver for me — just diagnosed with Hashi’s about 6 months ago. I’m curious about the D-ribose — I feel like it could be very helpful to me, but is it possible for it to trigger candida issues since it is a sugar? I feel like your electrolyte blend would help me a lot, but I’m still in the process of eradicating/rebalancing the candida in my gut — wondering if it would be better to wait until after that is resolved before taking D-ribose?