Years ago, I struggled just to get through each day. I had so many frustrating symptoms, including anxiety, irritable bowel syndrome (IBS) and acid reflux. I also had other seemingly odd symptoms for someone my age, like frequent muscle cramps, stiffness, carpal tunnel in both arms, and pain. (I’ve shared articles on pain and will be sharing one on carpal tunnel soon as well.)
Furthermore, no matter how much exercise I did, I wasn’t able to gain any muscle… and the muscle I previously had, seemed to waste away. While I didn’t realize this at the time, muscle wasting is indeed a symptom that is more common in those with thyroid issues. [1]
As I began the journey of taking back my health, the pain, cramps and stiffness subsided, while my muscle strength eventually returned to my previous baseline (though I have never considered myself to be a “bodybuilder”). In my own practice, many of my clients have had some form of muscle complaint, often involving muscle loss, muscle weakness, pain, and/or cramps. Interestingly, my male clients reported more muscle loss/weakness, while female clients reported more symptoms of pain, cramps, and weight gain.
Being a Root Cause detective, I learned that muscle weakness, pain and muscle loss were common symptoms for people with Hashimoto’s. Research has shown that as many as 80 percent of people with thyroid disorders also have muscle-related disorders. [2] Furthermore, some women may experience a loss of muscle after pregnancy.
For some, optimized thyroid hormone replacement therapy will be the answer, but others may need to dig deeper to address key root causes (especially nutrient deficiencies) that may lead to muscle issues.
So let’s talk about muscle wasting (sometimes known as muscle atrophy or sarcopenia, when it occurs in a person of advanced age).
In today’s article, we’ll cover:
- Why muscle wasting occurs
- The Hashimoto’s – muscle wasting connection
- The conventional treatment for muscle wasting
- The Root Cause approach to treating muscle wasting
- Specific steps to rebuild muscles (and feel better)
Hashimoto’s & Muscle Concerns
Muscle issues seen in Hashimoto’s can fall into more than one different category, including myopathies and muscle atrophy (sometimes known as sarcopenia in older individuals). There are similarities and differences between these forms of muscle issues, and sometimes they can overlap.
Myopathy is a broader term that refers to any disease that affects muscle tissue and results in weakness, inflammation, spasms, or paralysis. Most common are acute (or acquired) myopathies, such as stiffness, spasms, or cramping. Other forms of myopathies are linked to exposure to a virus or bacteria, or are inherited. Most commonly, people develop acquired myopathy from muscle fatigue or electrolyte imbalance, which results in stiffness or cramping. Other causes of myopathies include immune disorders that cause inflammation and pain.
It’s important to note that there may be additional causes of myopathies, such as mitochondrial myopathy, that may overlap with the muscle wasting or sarcopenia seen in Hashimoto’s. Studies have shown reduced mitochondrial oxidative enzyme activities in cases of sarcopenia and mitochondrial myopathy, but the reduction seems to be greater in those with sarcopenia. [3] In those with sarcopenia, reduced enzyme activity was observed on mitochondrial complexes I, II and III, while those with myopathy had reduced activity on complex IV, indicating that there are differences in the way these types of muscle conditions affect us on a cellular level.
Sarcopenia is a form of muscle wasting that most often occurs with aging and/or immobility. Although it is primarily a disease of the elderly, its development may be associated with conditions that are not exclusively seen in older persons, including hormone dysregulation. The primary characteristics are a loss of skeletal muscle mass, quality, and strength. Factors including exercise, comorbidities, and nutrition can influence the rate of muscle atrophy. To an extent, this type of muscle loss is normal, and adults begin losing approximately 3-8 percent of their muscle mass per decade, after the age of 30. [4]
The European Working Group on Sarcopenia in Older People (EWGSOP) relies on specific and easily identifiable parameters, such as muscle mass, strength, and physical performance, to diagnose the condition. They define sarcopenia as the presence of both low muscle mass and low muscle function (strength or performance) as measured by gait speed and assessment of grip strength. The EWGSOP also uses a grading scale for sarcopenia: pre-sarcopenia (decreased muscle mass with normal strength and physical performance), sarcopenia (decreased muscle mass with decreased strength or performance), and severe sarcopenia (decreased muscle mass, strength and performance).
Common symptoms seen in those with sarcopenia include: [5]
- Loss of lean muscle mass, especially in thighs and abdominal areas
- Weakness
- Reduced strength
- Increased risk of falling
These symptoms may be exacerbated by over-exertion, exercise, or cold temperatures.
While myopathy and sarcopenia related forms of muscle issues can occur in those with Hashimoto’s, this article will focus on muscle issues in the form of muscle wasting that is most similar to the sarcopenia seen in the elderly, as my clinical experience has shown it to be the most common form of muscle loss we observe in thyroid conditions. Because there are so many different ways to describe subtle variations of each muscle condition, I want to prevent confusion and will be referring to this condition as “muscle wasting.”
The Thyroid & Muscle Wasting Connection
Muscle wasting was common enough in my clinical practice that I routinely screened for muscle wasting symptoms during new client intakes. Interestingly, this was a symptom mainly noticed by men, who reported feeling weaker and less athletic, in contrast to women, who were more likely to notice excess weight gain and feel more “squishy.” Additional related issues that were commonly reported included pain, fibromyalgia and carpal tunnel. (I’ve written a bit about pain and fibromyalgia and will be writing a post on carpal tunnel syndrome soon. :-))
This came as no surprise, as muscle-related issues have been found to be more common in people with thyroid conditions.
In one Chinese study, researchers investigated the effect of thyroid hormones on body muscle mass, muscle strength, and physical function related to sarcopenia in elderly Chinese individuals with normal thyroid function. [6] After measuring thyroid hormone levels and muscle function through grip tests and physical function, it was concluded that those individuals with higher levels of free triiodothyronine (FT3) within normal ranges, had more muscle mass and greater muscle function.
In multiple studies, the frequency of neuromuscular complaints (including muscle weakness, neuropathy, and carpal tunnel) found in hypothyroid patients, has been shown to be between 20 to 80 percent. In one 2000 study, researchers found that 79 percent of patients with hypothyroidism (and 67 percent of those with hyperthyroidism) had muscle complaints, with 54 percent of those having muscle weakness and 42 percent having cramps. [7] Additionally, 25 percent had carpal tunnel syndrome.
One smaller study found that about 90 percent of people with hypothyroidism had proximal weakness of some kind. [8] This is a weakness closer to the body’s midline (versus further out on the limbs).
So why do muscle-related issues like muscle wasting occur so often in people with thyroid disease?
Why Muscle Wasting Occurs
Muscle wasting is a catabolic state of the body, when the body shunts resources away from building up our muscles and our muscles become weaker, instead of stronger. During muscle catabolism, the body begins to break down muscle protein to provide fuel to other functions.
People may notice that they don’t look as fit as they used to anymore, or they may have more difficulties with physical activities (such as intense physical exercise, and in some advanced cases, even light types of physical activities, such as walking). When a person is in a catabolic state, muscle mass tends to diminish and the percentage of body fat increases. The person may become what a college friend of my husband used to call “skinny fat.”
Additionally, when the body goes into a catabolic state, an individual can start to display even more symptoms beyond muscle wasting, including: fatigue, chronic pain, poor immune function (lingering infections), poor sleep, poor digestion (lack of nutrient absorption), cravings, depression, and anxiety.
The opposite of the catabolic state, is the much healthier anabolic state, or a state of protein building, where the body provides enough resources for proper growth and repair of muscles. People in a healthy anabolic state will feel fit, strong, and generally healthy.
Please note: If you’ve ever watched the news, you may have a negative association with the word “anabolic,” due to coverage of illegal performance enhancement drugs used among bodybuilders or professional athletes, who may have used “anabolic steroids.” Anabolic steroids are generally defined as testosterone, or molecules with a similar mechanism of action. While the body makes anabolic hormones naturally, and in some cases, bioidentical dosages can be prescribed safely to ensure that we are in a balanced anabolic state if we are deficient, there are great risks when the steroids are used in excessive doses to “bulk up,” as they push the body into a hyper anabolic state. This article will be focused on restoring a healthy anabolic state, not on how to use anabolic steroids (whether legally or illegally ;-)).
So with that said, let’s get back to muscle wasting and why it happens…
I believe that muscle wasting occurs when we have an increase in inflammation for any reason, and the adrenals begin to pump out the anti-inflammatory hormone cortisol to counterbalance this inflammation. At a certain point, the cortisol pathway becomes impaired and the person no longer releases enough cortisol to counter the inflammation, which will then go unchecked. Supporting optimal adrenal function and cortisol levels will help to counter the inflammation.
I have found that Hashimoto’s can be triggered by an overwhelmed stress response, sluggish digestive system, and overburdened detox pathways. Additionally, nutrient deficiencies, food sensitivities and chronic infections are often present. All of these factors will create a state of chronic inflammation, and contribute to a deficiency in protein and the key building blocks of muscles — amino acids.
The process of muscle wasting sometimes begins when a person contracts a gut pathogen, which leads to a malabsorption of nutrients and inflammation in the body.
Malabsorption will lead to poor levels of key nutrients, particularly protein and amino acids, such as carnitine (which is needed to build the body back up). The inflammation creates chronic stress within the body that results in the release of the anti-inflammatory hormone cortisol, which will eventually become depleted in the body.
This leads the body to “steal” pregnenolone (the mother hormone that produces cortisol, DHEA and testosterone) to make more cortisol, while less DHEA and testosterone are made.
A catabolic state occurs in response to this inflammatory stressor: the body responds by seeking to divert its energy resources to where it is needed, to repair itself and survive. The most available source for this needed energy is found in the body’s protein, and the majority of protein in the body is found in skeletal muscle. Protein from skeletal muscle is broken down and converted to glucose (sugar) to create needed energy to tame the inflammation.
While the body does naturally create new protein, in an inflammatory condition like Hashimoto’s, it will break down more protein than it produces. It will eventually resort to obtaining its needed protein via consuming skeletal muscle. Over time, a loss of lean body mass – and other muscle related symptoms – can occur.
To get the body back on track, we need to support it by optimizing thyroid hormone levels, providing the proper building blocks (protein and amino acids), and supporting gut health by aiding digestion. Next, we need to support the body’s production of DHEA and testosterone hormones. Finally, we need to address any potential infections that may be leading to the malabsorption (and sometimes Hashimoto’s too!). Eradicating infections can sometimes be done with a very simple beneficial yeast that boosts our own body’s defenses; in other times, deeper protocols may be required.
Of note, a catabolic state also occurs in late pregnancy to allow for more nutrients to become available to the baby. [9] I can attest to this personally, as towards the end of my pregnancy, I began to feel very weak, and had more frequent pain from everyday things, such as walking. I remember crying when my husband brought the car-seat home in fear that I wouldn’t be able to carry the car-seat and our son! After giving birth, I felt like I had no core strength… I was squishy and later developed a mom butt. 🙂 I know many women with Hashimoto’s say that they feel “stuck” in that squishy shape after pregnancy, and I believe this could be due to a nutrient depletion, and potentially an infection that occurred during pregnancy, as we all know pregnant women have lowered immunity.
I am not sure if my symptoms were excessive compared to other women, but it took me some time to build up my body and get back into an anabolic state, by using many of the strategies I discuss in this article. I am pleased to say that while no one will mistake me for a bodybuilder these days, my pre-pregnancy butt is back! I no longer have a flat butt, and as my sweet son Dimitry said, “Mommy has a really big butt.”
Conventional Medicine’s Answer to Muscle Wasting
If you voice concerns about muscle fatigue or have trouble with gaining muscle, you’re likely to be told by most conventionally-trained doctors that you’re just getting older, or that you need more exercise.
We know that muscle mass does decrease with age, but generally, people with chronic inflammatory conditions are more likely to experience it… and they see it earlier in life and/or with a quicker progression.
The primary treatment for muscle wasting is physical exercise, with a focus on strength training. While this can be a helpful part of a treatment regimen, it won’t address the root cause for people with Hashimoto’s, and, on its own, is unlikely to reverse the condition.
Muscle wasting can also be challenging for conventional practitioners to tackle without pulling out the prescription pad, as its symptoms can be subtle and non-specific. Often, pain meds or even antidepressants are prescribed, while other doctors may prescribe physical therapy.
Root Cause Approach to Muscle Wasting
The following steps fall into four major categories: optimizing thyroid hormones, focusing on amino acid/protein intake, balancing the adrenals, and reducing inflammation. They address common root causes for Hashimoto’s — and in particular — muscle wasting symptoms.
1. Optimize Thyroid Hormone Levels
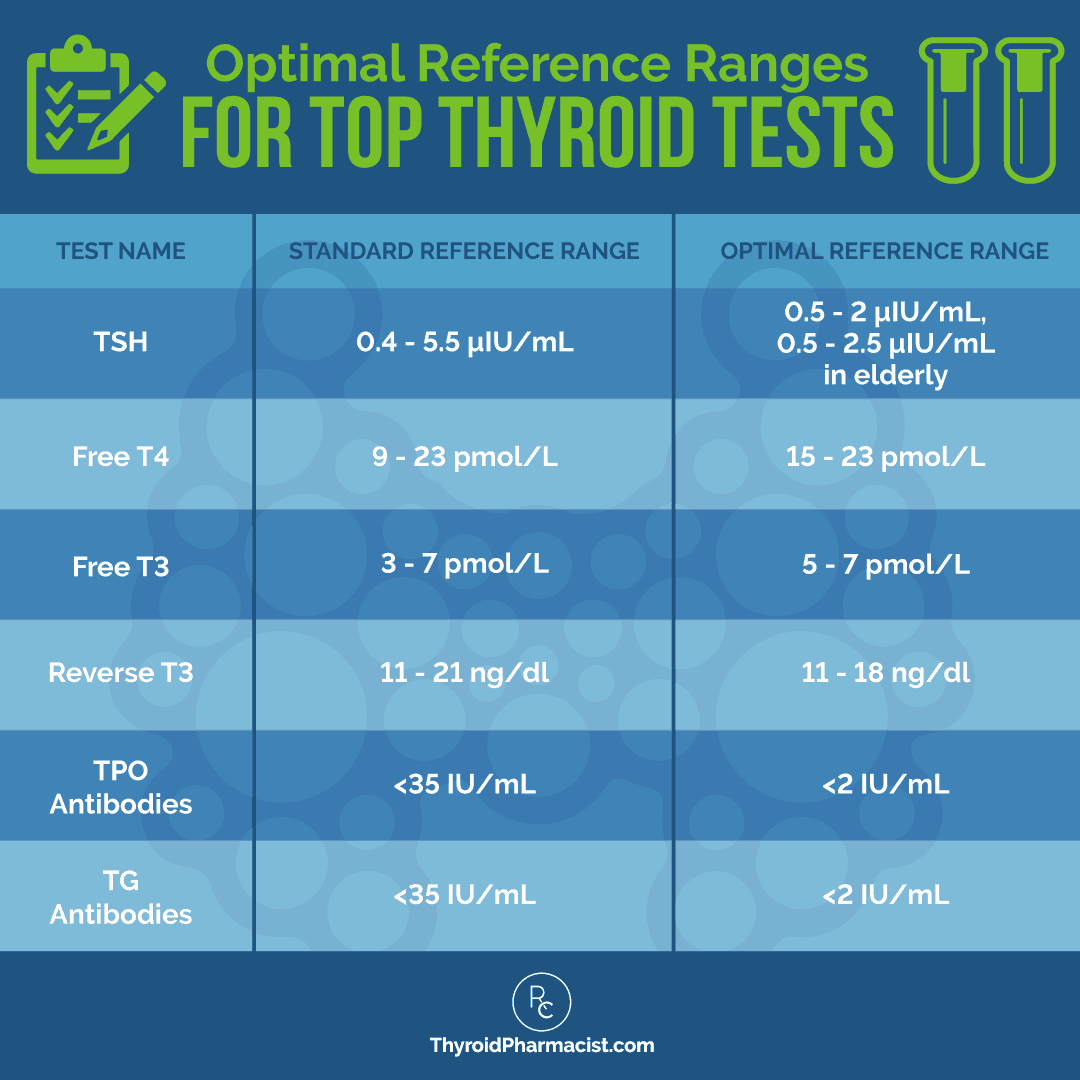
As a functional medicine practitioner and Root Cause detective, to me, an early diagnosis for Hashimoto’s is a vital first step to feeling better. For someone who has not yet been diagnosed, the first step to resolving muscle wasting (and many other health issues) would be thyroid antibody testing, along with a complete thyroid panel. We can often find thyroid antibodies years before a person’s TSH level tests as abnormal; and in all of that time, not only is there more thyroid damage likely occurring, but muscle wasting symptoms are also not getting addressed.
Thyroid hormones participate in numerous aspects of muscle development, including contractile function, metabolic processes, myogenesis and regeneration of skeletal muscle.
So first things first — if your muscle wasting is caused by inadequate levels of thyroid hormone, then you must optimize your thyroid hormone levels!
Studies have demonstrated that thyroid hormone levels can have an impact on muscle atrophy, as was observed in a 2015 study in Korea, which found that higher T4 levels were associated with sarcopenia in both men and women over the age of 60, when both gait speed and grip strength were measured. [10]
Using the Root Cause approach, we want to make sure that we have optimal TSH levels AND optimal T4 and T3 hormones, versus simply having TSH levels in the more conventional “normal” ranges. (You can read more about thyroid panels and optimal thyroid hormone levels here.)
If a client’s results are outside the optimal ranges, I may recommend a T4 or T4/T3 combination thyroid hormone replacement medication as a start. Research has shown that normalizing TSH levels (which thyroid medications can help with) may result in the improvement of symptoms related to muscle atrophy.
However, for some, the muscle wasting is NOT related to thyroid hormone levels at all. If your thyroid hormones are optimal, there may be additional steps that you will need to take to resolve muscle wasting. The good news is that many of these are easy to implement.
2. Focus on Getting More Building Blocks for Your Muscles
To get the body back on track, we will need to start by supporting it with the building blocks it needs — protein, amino acids, and digestive support — to properly break down and utilize the protein. We’ll also need to support the production of natural anabolic steroids by balancing cortisol levels, and eliminating any underlying infections.
Optimize Protein Intake
Remember, the body is breaking down its own muscle protein to fuel its inflammatory stress response. This means your overall requirement for protein will be increased. While we know that inflammation is at the root cause of this and we definitely want to address the inflammation (more on that in a minute) so that we no longer need as much protein, realistically, reducing inflammation to a healthy level may take some time.
In the meantime, we need to get adequate amounts of protein to build the body back up so that the inflammatory response isn’t leading to a breakdown of the muscle tissue. A key component of making sure that our muscles get the amino acids that they need to repair and build, is to ensure that we are getting enough of these amino acids into our system.
One obvious way to get more protein is to consume more protein. 🙂 Consider adjusting your diet to be more based on protein, and minimizing carbs and processed foods (this will also help your blood sugar, which is another key strategy for building muscles that I’ll speak to later in this article).
If you need some recipe ideas, you may want to look into the Paleo-style diet, which focuses largely on quality meats, vegetables, and fruits. (In my 2015 survey, 81 percent of my readers with Hashimoto’s said they felt better on this diet!)
When I started a Paleo diet, I remember feeling like, all of a sudden, my abs became more visible, even after years of being invisible and hidden despite hours and hours of abs and Pilates classes.
For more recipe inspiration, I suggest my book, Hashimoto’s Food Pharmacology: Nutrition Protocols and Healing Recipes to Take Charge of Your Thyroid Health. It’s chock full of delicious, nutritious, and thyroid-supporting recipes.
I also love to use protein powders in order to increase the amount of protein I’m ingesting. This is because they are already broken down and easy to incorporate into the day, in the form of smoothies and shakes. Be aware that most protein powders contain soy and whey, which are very reactive proteins for those with Hashimoto’s. [11] I recommend hydrolyzed beef protein and pea protein as the most hypoallergenic proteins for people with Hashimoto’s.
I created Rootcology AI Paleo Protein Powder and Vanilla Paleo Protein Powder (from hydrolyzed beef protein) specifically for people with Hashimoto’s. Surprisingly, beef protein is tasty and is less likely to cause food reactions due to the hydrolysis process (which breaks the protein into tiny pieces).
Rootcology Organic Pea Protein is another option I created, that is also less likely to be reactive. NOW Foods also makes a great pea protein powder.
I have also found hemp protein to be well tolerated by people with Hashimoto’s.
How much protein is needed?
- For general health purposes, you should be consuming about 0.45-0.55 grams of protein per day, for each pound that you weigh. This translates to roughly 50 grams of protein per day, for a person who weighs 100 pounds.
- Higher protein intake (0.55-0.68 grams per pound of body weight, per day) is recommended for most older adults who have acute or chronic diseases. In this case, a person who weighs 100 pounds should aim for 54-68 grams of protein per day.
- Generally, the more active you are, the more protein you need. Bodybuilders need even more protein — as much as 1 gram of protein per pound of body weight — so a 100 pound person would want to aim for 100 grams of protein each day!
- Older people with severe kidney disease (who are not on dialysis) are an exception to this rule — these individuals may need to limit their protein intake, as their kidneys may not be able to properly process the protein.
Support Protein Digestion
Another key point here is to ensure that we are DIGESTING our protein. People often say that we are what we eat. I agree, and would take it one step further and say, we are what we digest. 🙂 Low stomach acid levels that lead to protein malabsorption are very common in Hashimoto’s. [12] Taking a supplement like Betaine with Pepsin is going to be incredibly helpful for digesting protein.
Betaine with pepsin can make a tremendous difference in a person’s symptoms because, once we begin to digest our proteins correctly, a few great things can happen:
- The body may not need to expend as much energy on digestion, and since digestion is one of our body’s biggest energy expenditures, we often begin to have a surplus of energy.
- The amino acids found in proteins become bioavailable, helping with the creation of neurotransmitters and fuel for our bodies.
- We will be less likely to react to our foods, as the food particles will get broken down into individual amino acids before they move further down into our gut.
- We will feel lighter after we eat, and will not have cravings for food when full.
In general, the more protein and the more tightly the protein molecules are bound to one another, the more betaine and pepsin you’ll need to take with each meal. For example, a steak dinner would require more betaine and pepsin than a pea protein smoothie. 😉
As an additional benefit, betaine and pepsin can lead to reduced overall inflammation and pain for many people. [13] Betaine can break down homocysteine as well, which further reduces inflammation, and is especially helpful for those with MTHFR gene mutations.
Consider Carnitine Supplementation
Protein consists of 20 amino acid building blocks, nine of which the body has to take in through diet (as the body doesn’t make them). These nine essential amino acids are histidine, isoleucine, leucine, lysine, methionine, phenylalanine, threonine, tryptophan, and valine. We can generally get these from a whole foods-focused, Paleo-like diet that restricts processed foods; but diving into the research as well as my own lab testing, I have found that many people with Hashimoto’s are actually DEFICIENT in many of the amino acids — even the ones our body is “supposed” to make.
Carnitine is an amino acid found in abundance in skeletal muscle, and has traditionally been associated with muscle wasting in Graves’ disease, but has also recently been implemented in Hashimoto’s as well as in pregnant and newly postpartum women. This deficiency can lead to symptoms including fatigue, brain fog, constipation, digestive issues, and muscle weakness/aches.
Research has shown that, in hypothyroid patients, there was indeed a trend for muscle carnitine content to be lower than normal, and that carnitine levels improved with thyroid hormone treatment. [14] As a side bonus, carnitine supplementation studies have demonstrated an improvement of glucose tolerance in insulin-resistant states, in doses ranging from 1000 to 4000 mg. [15] This is important to note, as blood sugar balance is another key component of restoring muscle mass.
In my experience, supplementing with carnitine can be a game changer for muscle weakness in people with both Hashimoto’s and Graves’ disease.
I recommend Rootcology’s Carnitine Blend, which uniquely combines L-carnitine (for muscles) and acetyl-L-carnitine (great for brain function!) into one convenient 500 mg capsule. Therapeutic doses of 2 capsules, taken twice per day, can help restore carnitine levels in the body.
Additionally, I will often recommend amino acid support supplements such as Amino-NR (a wonderful complex of important amino acids, including the branched-chain amino acids that support muscle building), or Free Form Amino Caps.
3. Create More Natural Anabolic Steroids with Adrenal Support
Supporting our adrenals and reducing stress can help shift the body out of a catabolic state and back into an anabolic state, where muscle building can resume.
Our adrenals release hormones such as cortisol and the anabolic DHEA, which is often called our “youth hormone.” The main role of cortisol is to keep the body fueled during a stressful time. As mentioned earlier, cortisol shifts the body into a tissue-breakdown phase (catabolic) instead of a tissue-repair phase (anabolic). Under normal conditions, there is a balance between catabolic and anabolic phases.
Again, during stressful situations, the body shifts hormone production away from producing the hormones DHEA, progesterone, and testosterone, to focus on producing cortisol. This mechanism is known as “pregnenolone steal.” It is a protective way of conserving resources to help us survive stressful “fight-or-flight” situations, like being chased by bears. However, our stress response can turn on in non-life-threatening situations we find stressful, like running late or being stuck in traffic. This can then turn into a chronic activation of the stress response where the body works extra hard to keep producing more cortisol, stopping the production of other hormones normally produced by the adrenals (such as progesterone, DHEA, and testosterone).
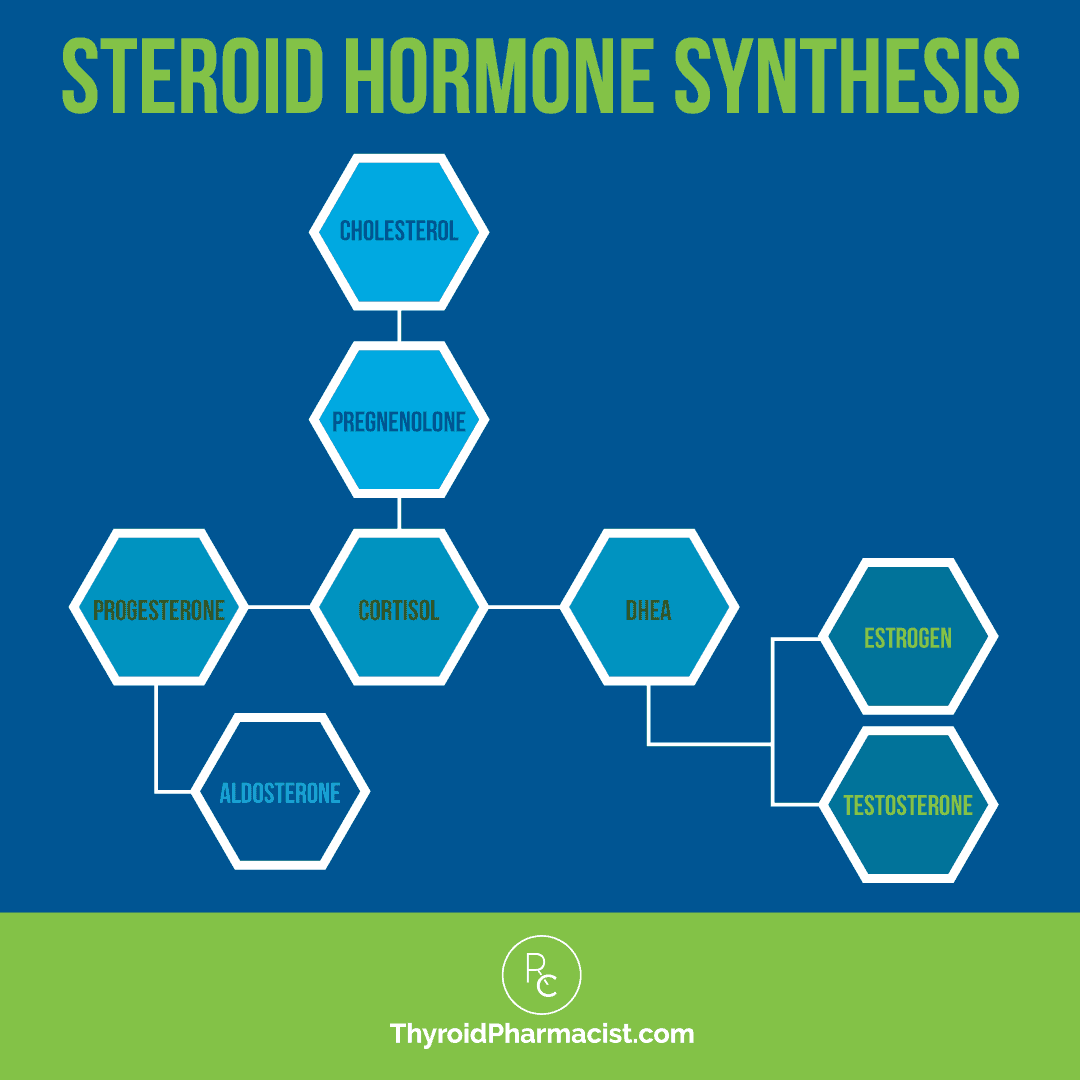
As an anabolic steroid, DHEA helps with tissue repair, counterbalancing the effects of cortisol. However, when DHEA becomes depleted during the chronic stress response, this can contribute to muscle loss.
To support the production of natural anabolic steroids (DHEA and testosterone) and get the body back into muscle-building mode, we need to balance our cortisol levels by supporting adrenal health.
This is the goal of the program outlined in my new book, Adrenal Transformation Protocol. Through simple shifts in our diet and lifestyle, we can support healthy cortisol levels naturally, and the production of DHEA and testosterone, without the need for supplemental hormones.
Support DHEA Levels
While DHEA supplements are available and may be recommended for some individuals, they should not be used without the guidance of a medical practitioner or without prior testing of DHEA levels.
Alternatively, magnesium supplements can help restore DHEA levels and are safely recommended for most people. [16] Magnesium can be taken in supplement form. It can also be applied topically — this form may be better absorbed by some people. Using 2-4 oz. in a bath or a foot soak is recommended to restore intracellular magnesium levels. Epsom salt baths have also been found to increase magnesium levels.
Adaptogens can help normalize DHEA levels as well. [17] I love adrenal adaptogens and have taken them on and off for many years (especially during periods of stress), although I did stop them during pregnancy (many can be used safely while nursing, but that is a separate article for the future). As an ultra-busy mom, I have started taking them again. A favorite of mine is maca, which contains muscle-supportive magnesium and amino acids. It can be a great addition to your regular protein drink!
I also developed my own adaptogen blend, Rootcology Adrenal Support, which contains a combination of adaptogens and vitamins to support DHEA levels and a healthy stress response.
Hydration and Electrolyte Balance
Maintaining proper hydration and electrolyte balance is another important step in supporting the adrenals and preventing muscle wasting, and is easy to tackle every day. The protein components that create muscle fibers are dependent on electrical forces to do their job of expanding and contracting, and are highly dependent on a proper pH balance — otherwise, muscle damage can occur. [18] An acidic state has been clinically associated with sore muscles, muscle cramps, spasms, tics, and restless legs. [19] Therefore, proper hydration and electrolyte balance are an important part of maintaining muscle health.
The general recommendation is 6 to 8 cups (or 6 to 8 eight ounce glasses) per day of clean, filtered water — but to get a precise amount specific for your body, there is a simple calculation that you can do.
In general, you will want to drink half your body weight (measured in pounds), in ounces. For example, a 150 pound person would aim to drink 75 ounces of water per day.
Depending on your activity level, however, you may find that you need more.
In addition to drinking water, it is also important to pay attention to your electrolyte balance.
Electrolytes are minerals that play a critical role in the body. Through a biochemical process, electrolytes become ions (an atom or molecule with an electrical charge) that can conduct electrical signals in the body. These signals create communication and function within nerves and muscles, as the electrolytes move in or out of cells. Electrolytes are important for fluid balance, muscle contraction, and blood pressure, and play other roles in the body as well.
Electrolytes include:
- Sodium
- Potassium
- Calcium
- Magnesium
- Chloride
- Phosphate
- Bicarbonate
Potassium is the main intracellular (inside the cell) ion, and sodium is the main extracellular (outside the cell) one. Potassium and sodium are arguably the most important for maintaining good hydration and electrolyte balance within the body. Sodium and potassium function in the body in a very specific balance.
You’ll notice that magnesium is also listed as an electrolyte. Magnesium deficiency is a root cause for a variety of muscle-related symptoms, including joint pain and muscle cramping.
A simple hack to remain alkaline (i.e. reduce our acidic state) and reduce muscle aches is to drink more water, add sea salt to the mix, and take Magnesium Citrate Powder by Rootcology (which also supports a better night’s sleep) or Magnesium Glycinate by Pure Encapsulations (which helps to repair and rebuild muscle), as well as a potassium bicarbonate supplement, such as K Alkaline by Moss Nutrition (which supports an alkaline state) at bedtime.
I also recommend adding in Rootcology Electrolyte Blend to help maintain a healthy electrolyte balance. This blend contains magnesium, potassium, sodium, and chloride, in addition to D-ribose, which is important in healthy cardiac function, exercise recovery, and energy production. In fact, D-ribose was recently studied for its ability to help athletes recover from strenuous exercise. [20] The athletes, who were given 10 g per day of D-ribose during high intensity training, showed significant improvements in performance and reduced levels of the muscle damage marker creatine kinase (CK), with a lowered perceived exertion reported on the part of the test participants.
For a more in-depth look at supporting your adrenals, I recommend checking out my newest book, Adrenal Transformation Protocol. It takes you through a simple four-week program to help identify your adrenal triggers, balance your stress response, and gradually build up your resilience to set you up with a strong foundation to support your adrenals now and in the future.
Balance Blood Sugar
Blood sugar imbalances are one of the top contributors to adrenal dysfunction, and insulin resistance has been associated with muscle wasting, as well as Hashimoto’s. In a 2017 study on insulin resistance and Hashimoto’s, the authors concluded that high thyroid antibody levels are related to high fasting blood glucose levels and high insulin levels. [21]
Dietary changes focus on removing excess carbs and adding protein and healthy fats with every meal, to stabilize blood sugar. Try not to exceed a 2:1 ratio of carbs to protein. Focusing on low glycemic index (GI) and low glycemic-loaded (GL) foods, which burn slower, can really help with balancing blood sugar. Read more about how to naturally address blood sugar and insulin issues here.
There are a variety of supplements that can help improve insulin sensitivity and balance blood sugar. A couple that I like to recommend include:
- L-Glutamine Powder by Pure Encapsulations: This form of glutamine (also found in bone broth) supports the mucosal lining and the healthy functioning of the gastrointestinal tract. [22] As an essential amino acid, it also supports lean muscle mass, especially in times of metabolic stress. Research has shown glutamine to be effective in restoring insulin response in diabetics. [23]
- Myo-Inositol Powder by Rootcology: Supplementation with this form of inositol has been shown to have many benefits for Hashimoto’s, including improvements to insulin sensitivity, as well as lowered thyroid antibody and TSH levels (when taken in conjunction with selenium). [24]
Further lifestyle interventions that can help support the adrenals include a focus on better sleep habits and stress management. (Learn more about supporting your adrenals and improving your sleep habits.)
4. Reduce Inflammation
As chronic inflammation can cause protein deficiency, it’s important to address the root causes of it. We know that inflammation drives the body to produce more cortisol, and we can spare some cortisol by lowering inflammation and using additional anti-inflammatory products.
The top root causes of inflammation in the body include food sensitivities, chronic gut infections, and certain nutrient deficiencies.
Eliminate Food Sensitivities
Food sensitivities can cause inflammation and lead to an impaired ability to extract the nutrients we need from the food we eat — including amino acids — to properly build and maintain muscle mass.
Based on my clinical experience and survey of over 2000 people with Hashimoto’s, the most common food sensitivities found in people with Hashimoto’s are gluten, dairy, soy, grains (corn, in particular), nightshades (potatoes, tomatoes, and peppers), nuts, and seeds.
In surveying my readers and clients, I’ve found that about 93 percent have felt better on a gluten-free diet. Another 75 percent reported feeling better on a dairy-free diet, 73 percent felt better grain free, and another 60 percent said they felt better soy free. Egg and nightshade free diets were helpful 40 percent and 35 percent of the time, respectively.
My personal and clinical experience has shown that gluten sensitivity is one of the most significant triggers in Hashimoto’s, and most people experience significant health improvements when they remove gluten from their diets. In fact, removing gluten can help reverse intestinal permeability (which is always a precursor to autoimmune disease), as well as reduce one’s thyroid antibody levels! [25]
The best place to start when trying to identify your own particular food sensitivities, is with an elimination diet. The first step will be to remove gluten, dairy, soy, and other foods that you suspect you may be reactive to. These may include fruits and vegetables you’ve been eating all the time. Avoid these foods completely for at least two weeks. During this time, make note of your symptoms. Which have improved? Which still remain?
After you have spent a period of two weeks without the suspected food irritants, try slowly adding them back in one at a time, waiting several days between each food to notice if any of your symptoms return. Many people will notice an immediate reaction when they reintroduce a food they are sensitive to. If you experience this, take this as a very strong clue that you should avoid that food!
For harder-to-identify food sensitivities, I recommend the Alletess lab test, which can be ordered through your primary care practitioner. If you prefer to order the home test kit, MyMedLab offers two options to test for the most commonly eaten foods: the 184 Food Panel and the 96 Food Panel.
Heal the Gut
In addition to food sensitivities, various pathogens like Blasto and H. pylori as well as overgrowths of normal flora seen in cases of SIBO or Candida infections, can cause gut inflammation and lead to protein malabsorption issues. [26]
S. boulardii, a beneficial yeast, can be very helpful for clearing out these pathogens, which in turn allows for gut healing and better absorption of nutrients. I recommend starting with two capsules per day, and slowly moving up to a therapeutic dose of as many as two capsules, three times per day.
Adding in a quality probiotic daily, such as Rootcology ProB 50, may also help improve your gut health, as a gut microbiome that is out of balance can lead to intestinal permeability. [27]
Also known as leaky gut, intestinal permeability occurs when the tight junctions that form the lining of the intestines become damaged and loose. This allows toxic substances to become absorbed into the bloodstream, causing the body to recognize them as foreign invaders. This then causes inflammation in the body as it begins to attack the intruders, and eventually leads to autoimmunity. [28]
There are numerous factors that can cause intestinal permeability, including adrenal fatigue, alcohol, dysbiosis, enzyme deficiencies, food sensitivities, gut infections, nonsteroidal anti-inflammatory drugs (NSAIDs), nutrient depletions, and various toxins.
To learn more about how to address the root causes of intestinal permeability, I encourage you to take a look at my article on gut health.
We may also want to add in a few other micronutrients that can aid the body’s rebuilding process, especially with a few nutrients that many people with Hashimoto’s are found to be deficient in. I often recommend L-glutamine and zinc to clients, to support healthy digestion.
- L-glutamine is usually depleted in people with Hashimoto’s and chronic stress. [29] As mentioned earlier, this amino acid is essential to proper gut lining and immune function, and can help tighten the intestinal junctions, which allows the gut to heal and nutrients to be better absorbed. L-glutamine was shown to reduce intestinal permeability in subjects with Crohn’s disease. [30] L-glutamine is dosed daily at 0.5 grams of glutamine per kilogram of ideal body weight.**To calculate your ideal body weight (IBW), use the following formula:
Males: IBW = 50 kg + 2.3 kg for each inch over 5 feet
Females: IBW = 45.5 kg + 2.3 kg for each inch over 5 feet
- Zinc is another key nutrient that I often recommend supplementing with, as zinc deficiency can be the result of a low protein diet or a diet rich in phytates (compounds found in whole grains, nuts, and seeds that can render zinc non-absorbable in the body). Zinc deficiency is also a common side-effect of toxic medications such as PPIs (proton pump inhibitors), and is often a trigger for leaky gut. [31] I usually recommend doses of no more than 30 mg per day, unless you’re working with a practitioner who advises higher doses. To ensure proper absorption, zinc supplements should be taken with food.
Additional Supplements to Help Reduce Inflammation
Certain nutrients and enzymes can support anti-inflammatory responses within the body and help with reducing inflammation. As an added bonus, they’re likely to reduce any muscle pain you may have! A few that I recommend include:
- Omega-3 Fatty Acids: These fatty acids help with symptoms and conditions associated with inflammation such as pain, intestinal permeability and muscle aches. Research has found that compared with over-the-counter ibuprofen, omega-3 fatty acids equally reduced arthritic pain, and were a much safer alternative for long-term pain reduction. [32] Here are some of the omega-3 supplements that I recommend:
- EPA/DHA Essentials by Pure Encapsulations, 2 capsules per day with food
- OmegAvail™ Synergy by Designs For Health, 2 capsules per day with food
- Arctic Cod Liver Oil by Nordic Naturals, one teaspoon daily
- Turmeric (curcumin is the active component): This a great natural pain and anti-inflammatory choice that can be helpful in down-regulating autoimmune conditions, reducing joint inflammation, and providing anti-inflammatory support for a variety of gastrointestinal conditions. [33] It can also help detoxify the body from heavy metals. [34] You can add turmeric to your favorite recipes, or take 1 capsule per day of Rootcology Curcumin Absorb for anti-inflammatory support.
- Systemic Enzyme Complex by Pure Encapsulations: These enzymes support muscle and joint health, and speed up tissue repair by reducing inflammation. Proteolytic enzymes have also been found to support muscle comfort and recovery of contractile function, as indicated in one placebo-controlled human study involving athletes. [35] Take 2 capsules, 1-2 times per day, between meals.
- Vitamin D: While vitamin D is well known to help support bone mass density and lower the rate of bone loss, it also helps maintain muscle fiber structure and function. [36] (Low levels of vitamin D are associated with lower muscle strength, increased body instability, falls, and disability in older adults.) [37] Vitamin D also has anti-inflammatory properties and has been studied to reduce muscular pain. [38] As the recommended daily allowance of 400 IU of vitamin D has been shown to be inadequate for most people, I generally recommend 5,000 IU per day as a starting point for my clients with Hashimoto’s. Taking vitamin D supplements with a meal can be helpful in increasing its absorption by 30-50 percent. However, I also recommend monitoring vitamin D levels to ensure that you are within the optimal range (60 to 80 ng/mL for optimal thyroid receptor and immune system function).
What About Exercise?
Too much intense exercise, without replenishment, can lead to further muscle loss and be counterproductive to your goals. However, the right amount and type of exercise, supported by diet and targeted supplements, can help shift the body into an anabolic state where we are once again building muscle.
Try some simple muscle training activities. These restore balance between the breaking down (catabolic) and building up (anabolic) processes that occur in the body. To get started, I recommend the following gentle muscle-building exercises, one to three times per week:
- Yoga: This gentle activity has a big focus on breathing, mindfulness, and stretching. (Yoga is an excellent exercise for stress reduction, too!)
- Pilates: This exercise works to recondition and realign the body, improving our posture and the way we move our muscles, leading to a gradual strengthening and toning of the body.
- Weight training: Lifting weights helps to build up muscle by putting the body into “anabolic build-up” mode. As a general rule, you should only do exercises that make you feel better. If you feel more tired after exercising, this means that your adrenals are not yet ready for it (if you are exercising too hard, you are likely increasing your cortisol levels). If things worsen with even gentle exercise, there may be a need for additional adrenal support.
You may be wondering, what about more intensive activities like aerobic exercises? Aerobic exercises that increase our heart rate (such as biking, running, and step classes) can actually worsen the catabolic process. I believe that aerobic exercise is great, but we have to be strong enough to perform it. Too much strain will result in muscle breakdown. One of my mentors, Dr. Dan Kalish, always says that he lifts weights so that he can be strong enough to spend many hours biking. Again, only do exercises that make you feel better. Know your body’s limits and make sure you do not overwhelm it!
Choosing the right type of exercise is something I discuss in my new book, Adrenal Transformation Protocol. In addition to exercise, it provides you with a simple four-week program to support your adrenals and build your body back up, so that you can be resilient enough to do the exercise you enjoy, and have energy for everything else in your life.
The Takeaway
Muscle wasting related to muscle atrophy, also known as sarcopenia, is often an overlooked condition, and most people don’t think of the thyroid being at the root of it — but it is a common symptom of those with Hashimoto’s. Sometimes it’s related to thyroid levels — other times, to protein deficiency.
If you are experiencing issues related to muscle wasting, the good news is that, in many cases, just starting or optimizing thyroid hormone replacement therapy may improve your symptoms. If you have muscle issues and haven’t yet been diagnosed with a thyroid condition, a good first step would be to get your thyroid antibodies tested.
If you already have a diagnosis, start digging for and addressing the root cause of your muscle wasting. Remember to do the simple things first… focus on increasing your muscles’ building blocks by bumping up your protein consumption, aiding protein digestion, and supplementing with key nutrients, such as carnitine. Next, support adrenal health to balance hormone production and help the body get back into an anabolic state, where it can build muscle tissue.
Then, work to reduce inflammation by identifying food sensitivities and supporting your gut health, which may involve using S. boulardii to clear out pathogens that may be at the root of your symptoms. Consider adding in a few supplements to help reduce inflammation, such as L-glutamine, vitamin D, systemic enzymes, and fatty acids, as well.
Finally, add in appropriate levels of exercise (don’t overdo it!).
To jumpstart you on a more Root Cause-supportive diet today (removing reactive foods and carbs, while providing optimal quality protein and fats), check out my cookbook, Hashimoto’s Food Pharmacology: Nutrition Protocols and Healing Recipes to Take Charge of Your Thyroid Health!
There are also some companies that I love that help ensure the highest quality protein makes it to your family’s dinner table:
- Vital Choice – Wild seafood and organic fare, harvested the right way.
- Butcher Box – High-quality meats delivered right to your door! (Use my code THYROID to get $10 off your order!)
- US Wellness Meats – Healthy meat options from properly fed animals.
- Paleo On The Go – Delicious ready-to-serve Paleo-friendly meals — all you have to do is heat them!
- Paleo Valley Grass Fed Beef Sticks – Protein-containing snacks that are perfect for when you need something quick and easy (and for travel).
I hope this helps, and wish you all the best on your healing journey!
P.S. You can download a free Thyroid Diet Guide, 10 thyroid-friendly recipes, and the Nutrient Depletions and Digestion chapter of my first book for free by signing up for my newsletter. You will also receive occasional updates about new research, resources, giveaways, and helpful information.
For future updates, make sure to follow us on Facebook, Instagram, TikTok, and Pinterest!
I love hearing from our community (and don’t forget to share your story relating to your own Hashimoto’s journey).
References
[1] Bloise FF, Oliveira TS, Cordeiro A, Ortiga-Carvalho TM. Thyroid hormones play a role in sarcopenia and myopathies. Front Physiol. 2018;9:560. Published 2018 May 23. doi:10.3389/fphys.2018.00560
[2] Duyff RF, Van den Bosch J, Laman DM, et al. Neuromuscular findings in thyroid dysfunction: a prospective clinical and electrodiagnostic study. Journal of Neurology, Neurosurgery & Psychiatry. 2000;68:750-755. doi:10.1136/jnnp.68.6.750
[3] Pestronk A, Keeling R, Choksi R. Sarcopenia, age, atrophy, and myopathy: Mitochondrial oxidative enzyme activities. Muscle Nerve. 2017;56(1):122-128. doi:10.1002/mus.25442; Marzetti E, Calvani R, Cesari M, et al. Mitochondrial dysfunction and sarcopenia of aging: from signaling pathways to clinical trials. Int J Biochem Cell Biol. 2013;45(10):2288-2301. doi:10.1016/j.biocel.2013.06.024
[4] Volpi E, Nazemi R, Fujita S. Muscle tissue changes with aging. Curr Opin Clin Nutr Metab Care. 2004;7(4):405-410. doi:10.1097/01.mco.0000134362.76653.b2
[5] Santilli V, Bernetti A, Mangone M, Paoloni M. Clinical definition of sarcopenia. Clin Cases Miner Bone Metab. 2014;11(3):177-180.
[6] Sheng Y, Ma D, Zhou Q, Wang L, Sun M, Wang S, Qi H, Liu J, Ding G, Duan Y. Association of thyroid function with sarcopenia in elderly Chinese euthyroid subjects. Aging Clin Exp Res. 2019 Aug;31(8):1113-1120. doi: 10.1007/s40520-018-1057-z. Epub 2018 Oct 26. PMID: 30367448.
[7] Duyff RF, Van den Bosch J, Laman DM, et al. Neuromuscular findings in thyroid dysfunction: a prospective clinical and electrodiagnostic study Journal of Neurology, Neurosurgery & Psychiatry 2000;68:750-755. doi:10.1136/jnnp.68.6.750
[8] Sharma V, Borah P, Basumatary LJ, Das M, Goswami M, Kayal AK. Myopathies of endocrine disorders: A prospective clinical and biochemical study. Ann Indian Acad Neurol. 2014;17(3):298-302. doi:10.4103/0972-2327.138505
[9] Lain KY, Catalano PM. Metabolic changes in pregnancy. Clin Obstet Gynecol. 2007;50(4):938–948. doi:10.1097/GRF.0b013e31815a5494.
[10] Choi YJ, Lee Y, Kim KM, Park S, Chung YS. Higher free thyroxine levels are associated with sarcopenia in elderly Koreans. Osteoporosis and Sarcopenia. https://doi.org/10.1016/j.afos.2015.11.001.
[11] Messina M, Redmond G. Effects of soy protein and soybean isoflavones on thyroid function in healthy adults and hypothyroid patients: a review of the relevant literature. Thyroid. 2006;16(3):249-258. doi:10.1089/thy.2006.16.249; Asik M, Gunes F, Binnetoglu E, et al. Decrease in TSH levels after lactose restriction in Hashimoto’s thyroiditis patients with lactose intolerance. Endocrine. 2014;46(2):279-284. doi:10.1007/s12020-013-0065-1
[12] Ebert EC. The thyroid and the gut. J Clin Gastroenterol. 2010;44(6):402-406. doi:10.1097/MCG.0b013e3181d6bc3e
[13] Zhao G, He F, Wu C, et al. Betaine in Inflammation: Mechanistic Aspects and Applications. Front Immunol. 2018;9:1070. Published 2018 May 24. doi:10.3389/fimmu.2018.01070
[14] Benvenga S, Amato A, Calvani M, Trimarchi F. Effects of carnitine on thyroid hormone action. Ann N Y Acad Sci. 2004;1033:158-167. doi:10.1196/annals.1320.015
[15] Ringseis R, Keller J, Eder K. Role of carnitine in the regulation of glucose homeostasis and insulin sensitivity: evidence from in vivo and in vitro studies with carnitine supplementation and carnitine deficiency. Eur J Nutr. 2012;Feb;51(1):1-18.
[16] Farsinejad-Marj M, Azadbakht L, Mardanian F, Saneei P, Esmaillzadeh A. Clinical and Metabolic Responses to Magnesium Supplementation in Women with Polycystic Ovary Syndrome. Biol Trace Elem Res. 2020;196(2):349-358. doi:10.1007/s12011-019-01923-z
[17] Lopresti AL, Drummond PD, Smith SJ. A Randomized, Double-Blind, Placebo-Controlled, Crossover Study Examining the Hormonal and Vitality Effects of Ashwagandha (Withania somnifera) in Aging, Overweight Males. Am J Mens Health. 2019;13(2):1557988319835985. doi:10.1177/1557988319835985
[18] Yu-Yahiro JA. Electrolytes and their relationship to normal and abnormal muscle function. Orthop Nurs. 1994;13(5):38-40. doi:10.1097/00006416-199409000-00008
[19] Law LAF, Sluka KA, McMullen T, Lee J, Arendt-Nielsen L, Graven-Nielsen T. Acidic buffer induced muscle pain evokes referred pain and mechanical hyperalgesia in humans. Pain. 2008;140(2):254-264. doi:10.1016/j.pain.2008.08.014
[20] Seifert JG, Brumet A, St Cyr JA. The influence of D-ribose ingestion and fitness level on performance and recovery. J Int Soc Sports Nutr. 14, 47 (2017). https://doi.org/10.1186/s12970-017-0205-8.
[21] Ceyhun V, Tezcan K, Perihan V, et al. Insulin resistance in the patients with euthyroid Hashimoto thyroiditis. Biomedical Research. 2017;28(4).
[22] Wang B, Wu G, Zhou Z, et al. Glutamine and intestinal barrier function. Amino Acids. 2015;47(10):2143-2154. doi:10.1007/s00726-014-1773-4
[23] Jafari-Vayghan H, Varshosaz P, Hajizadeh-Sharafabad F, et al. A comprehensive insight into the effect of glutamine supplementation on metabolic variables in diabetes mellitus: a systematic review. Nutr Metab (Lond). 2020;17:80. Published 2020 Sep 25. doi:10.1186/s12986-020-00503-6
[24] DiNicolantonio JJ, H O’Keefe J. Myo-inositol for insulin resistance, metabolic syndrome, polycystic ovary syndrome and gestational diabetes. Open Heart. 2022;9(1):e001989. doi:10.1136/openhrt-2022-001989; Nordio M, Basciani S. Myo-inositol plus selenium supplementation restores euthyroid state in Hashimoto’s patients with subclinical hypothyroidism. Eur Rev Med Pharmacol Sci. 2017;21(2 Suppl):51-59.
[25] Caio G, Lungaro L, Segata N, et al. Effect of Gluten-Free Diet on Gut Microbiota Composition in Patients with Celiac Disease and Non-Celiac Gluten/Wheat Sensitivity. Nutrients. 2020;12(6):1832. Published 2020 Jun 19. doi:10.3390/nu12061832; Fasano A. All disease begins in the (leaky) gut: role of zonulin-mediated gut permeability in the pathogenesis of some chronic inflammatory diseases. F1000Res. 2020;9:F1000 Faculty Rev-69. Published 2020 Jan 31. doi:10.12688/f1000research.20510.1; Krysiak R, Szkróbka W, Okopień B. The Effect of Gluten-Free Diet on Thyroid Autoimmunity in Drug-Naïve Women with Hashimoto’s Thyroiditis: A Pilot Study. Exp Clin Endocrinol Diabetes. 2019;127(7):417-422. doi:10.1055/a-0653-7108
[26] Ensari A. The Malabsorption Syndrome and Its Causes and Consequences. Pathobiology of Human Disease. 2014;1266-1287. doi:10.1016/B978-0-12-386456-7.03804-1
[27] Chakaroun RM, Massier L, Kovacs P. Gut Microbiome, Intestinal Permeability, and Tissue Bacteria in Metabolic Disease: Perpetrators or Bystanders?. Nutrients. 2020;12(4):1082. Published 2020 Apr 14. doi:10.3390/nu12041082
[28] Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol. 2012;42(1):71-78. doi:10.1007/s12016-011-8291-x
[29] Parry-Billings M, Dimitriadis GD, Leighton B, et al. Effects of hyperthyroidism and hypothyroidism on glutamine metabolism by skeletal muscle of the rat. Biochem J. 1990;272(2):319-322. doi:10.1042/bj2720319; Fürst P, Albers S, Stehle P. Stress-induced intracellular glutamine depletion. The potential use of glutamine-containing peptides in parenteral nutrition. Beitr Infusionther Klin Ernahr. 1987;17:117-136.
[30] Akobeng AK, Elawad M, Gordon M. Glutamine for induction of remission in Crohn’s disease. Cochrane Database Syst Rev. 2016;2:CD007348. Published 2016 Feb 8. doi:10.1002/14651858.CD007348.pub2
[31] Skrovanek S, DiGuilio K, Bailey R, et al. Zinc and gastrointestinal disease. World J Gastrointest Pathophysiol. 2014;5(4):496-513. doi:10.4291/wjgp.v5.i4.496
[32] Maroon JC, Bost JW. Omega-3 fatty acids (fish oil) as an anti-inflammatory: an alternative to nonsteroidal anti-inflammatory drugs for discogenic pain. Surg Neurol. 2006;65(4):326-331. doi:10.1016/j.surneu.2005.10.023
[33] Hewlings SJ, Kalman DS. Curcumin: A Review of Its Effects on Human Health. Foods. 2017;6(10):92. Published 2017 Oct 22. doi:10.3390/foods6100092
[34] Agarwal R, Goel SK, Behari JR. Detoxification and antioxidant effects of curcumin in rats experimentally exposed to mercury. J Appl Toxicol. 2010;30(5):457-468. doi:10.1002/jat.1517
[35] Marzin T, Lorkowski G, Reule C, et al. Effects of a systemic enzyme therapy in healthy active adults after exhaustive eccentric exercise: a randomised, two-stage, double-blinded, placebo-controlled trial. BMJ Open Sport Exerc Med. 2017;2(1):e000191. Published 2017 Mar 12. doi:10.1136/bmjsem-2016-000191
[36] Laird E, Ward M, McSorley E, Strain JJ, Wallace J. Vitamin D and bone health: potential mechanisms. Nutrients. 2010;2(7):693-724. doi:10.3390/nu2070693
[37] Aspell N, Laird E, Healy M, Lawlor B, O’Sullivan M. Vitamin D Deficiency Is Associated With Impaired Muscle Strength And Physical Performance In Community-Dwelling Older Adults: Findings From The English Longitudinal Study Of Ageing. Clin Interv Aging. 2019;14:1751-1761. Published 2019 Oct 15. doi:10.2147/CIA.S222143
[38] Wu Z, Malihi Z, Stewart AW, Lawes CM, Scragg R. The association between vitamin D concentration and pain: a systematic review and meta-analysis. Public Health Nutr. 2018;21(11):2022-2037. doi:10.1017/S1368980018000551
Note: Originally published in May 2021, this article has been revised and updated for accuracy and thoroughness.


 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
I find Dr Wentz articles like this one amazingly informative and practical. As someone with chronic Hashimoto’s, negotiating and making health decisions among the overwhelming amount of (often conflicting) information available today, can cause setbacks health wise, financially or otherwise. Dr Wentz takes the guesswork out of many of these complicated Hashi topics and provides unbiased useful advice. I always look forward to reading these in depth articles. Thank you
Tom – Thank you so much for your support! ❤️
You are so awesome and informative – have learned so much – so very helpful!!
Helena – thank you so much! ❤️
What would be the best supplement to start with I seem to identify with each thing you discussed
Kim – thank you for reaching out.❤️ Start with the simple things first, focus on increasing your muscles’ by increasing your protein consumption, aiding protein digestion, and supplementing with key nutrients, such as carnitine. Supporting adrenal health to balance hormone production and help the body get back into an anabolic state, where it can build muscle tissue is also important. The next step, work on reducing inflammation by identifying food sensitivities and supporting your gut health, which may involve using S. boulardii to clear out pathogens that may be at the root of your symptoms. Consider adding in a few supplements to help reduce inflammation, such as L-glutamine, vitamin D, systemic enzymes, and fatty acids, as well. Finally, add in appropriate levels of exercise (don’t overdo it!). I hope this helps.
Hola tengo hipotiroidismo ago exercicio y por más que ago no aumento masa muscular ,tomo levotiroxina de 88mg ,cómo puedo comprar los productos que recomiendan en este escrito ,por favor si me pueden ayudar ,gracias
Luz maria – thank you so much for following!❤️ Unfortunately, we cannot currently sell or ship our Rootcology supplements outside of the United States due to complicated regulations. Please email my team at info@thyroidpharmacist.com and they will be happy to share my international alternative supplements.
Thank you for your article. Can you recommend a holistic practitioner in nyc?
Amy – thank you for following. I believe that everyone needs to find a practitioner that will let them be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://bruno-michael-wentz.dev01.rmkr.net/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://bruno-michael-wentz.dev01.rmkr.net/database-recommended-compounding-pharmacies/