I often get messages from people with Hashimoto’s and other autoimmune diseases, that say: “Thanks for your efforts, but I’ve already tried everything. I have cut out gluten, dairy, and soy from my diet, and still have Hashimoto’s. How can your website and books help me?”
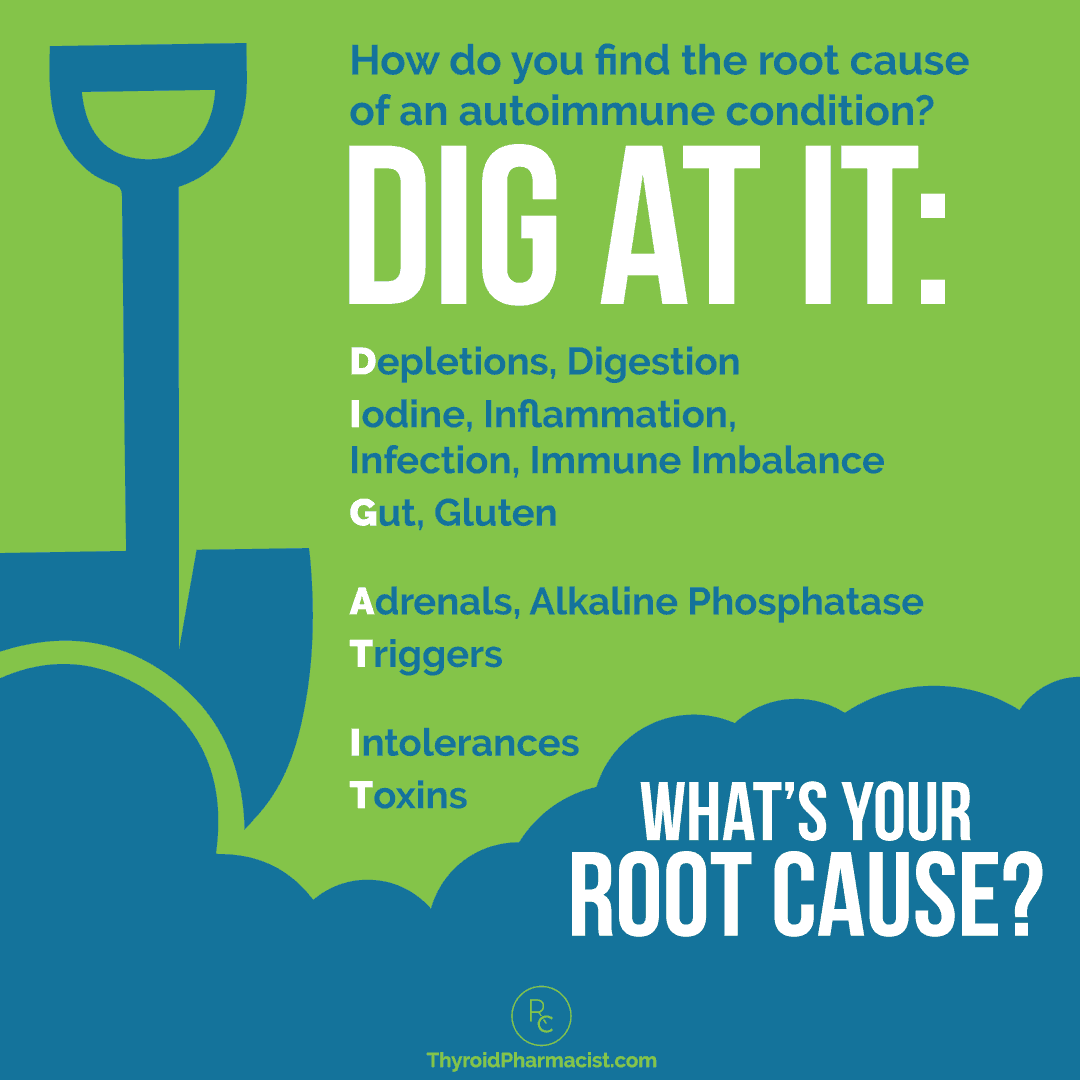
While changing your diet is an incredibly important first step that will greatly help many of you, if you do not see a complete remission of your symptoms within three to six months, I encourage you to dig deeper. Changing my diet was an important step in my healing journey, but it was just the beginning of it.
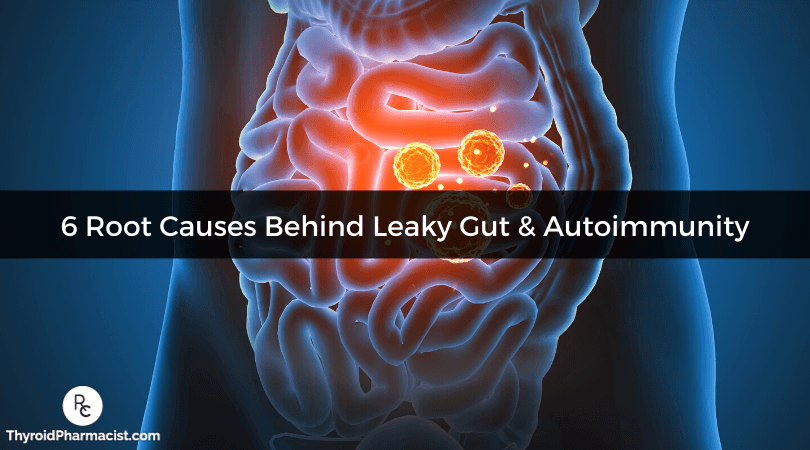
Everyone with autoimmunity, including those with Hashimoto’s, will experience some degree of intestinal permeability (also known as leaky gut). Healing a leaky gut can be a total game changer in getting Hashimoto’s into remission and resolving many of the associated symptoms.
The root causes of intestinal permeability are not the same from person to person. That said, I have seen several common root cause triggers time and time again, in those with Hashimoto’s. Based on my research over the years, I’d like to share six potential root causes of intestinal permeability with you. (There are, of course, many additional root causes, but these six are a great place to start.) Once addressed, many people are able to put their autoimmune thyroid disease into remission!
In this article, I’ll discuss:
- Six root causes of intestinal permeability (that contribute to Hashimoto’s)
- Ways to heal the intestinal lining
- How to address gut infections
Intestinal Permeability and Hashimoto’s
Dr. Alessio Fasano, world-renowned gastroenterologist and gluten intolerance expert, describes autoimmunity as a three-legged stool that needs three things to be present, in order to manifest:
- The right genes
- Exposure to a trigger, such as trauma, stress, toxins, the use of certain medications, and/or exposure to an antigen (any substance that induces the immune system to produce antibodies against it)
- Intestinal permeability (leaky gut)
With a chronic condition like Hashimoto’s, intestinal permeability occurs when the tight junctions within the intestinal wall start separating, and “holes” are created. These holes allow for food molecules, such as gluten, to pass through, and the body labels these molecules as foreign invaders. The body then launches an attack on these “foreign” molecules as well as the thyroid gland, as it is structurally similar to gluten.
While we can’t change our genes, we can reverse an autoimmune condition by removing the trigger(s) that contributed to its development, and by healing intestinal permeability. (You can read more about reversing autoimmunity in this article.)
Dr. Fasano often uses the example of celiac disease to explain this phenomenon. Celiac disease is a unique autoimmune condition where gluten acts as both the trigger and the cause of intestinal permeability! Once gluten is removed, the body is able to heal and regenerate itself.
Many gut-related issues, such as pathogenic infections, have been implicated as triggers in cases of autoimmunity, as well as contributors of a leaky gut.
As such, healing a leaky gut will also allow many individuals to put their condition into remission, as the “three-legged stool” of autoimmunity will no longer be able to stand!
What does this entail for those with Hashimoto’s? It entails healing the intestinal lining and helping those tight junctions stay tight, by removing dietary triggers such as food sensitivities, addressing nutrient deficiencies, restoring healthy zinc and glutamine levels, promoting healthy flora in the gut with pre- and probiotics where necessary, and eliminating any gut infections.
Let’s take a look at the most common root causes of intestinal permeability that I see in Hashimoto’s, and how we can address each of them.
Root Cause #1: Gluten Sensitivity
Gluten sensitivity may be the sole root cause, or it may be one of a few root causes, of autoimmunity, and has been implicated in various autoimmune conditions ranging from Hashimoto’s and Graves’ disease, to rheumatoid arthritis. It has been estimated that gluten may be a trigger for up to 20 percent of individuals with an autoimmune condition. Additionally, the prevalence of an autoimmune thyroid disease in those with celiac disease, is four times greater compared to the general population.
Exposure to gluten (specifically, the gliadin proteins that make up gluten) from gluten-containing foods can alter the properties of the cells that make up the intestinal barrier and, thus, weaken the structure of the barrier. (This happens even in those who do not have celiac disease.) This allows for gluten to “leak” into the bloodstream, and can lead to gut-related reactions associated with gluten sensitivity.
If an individual continues to consume gluten, this can contribute to the development of leaky gut, and increase its severity.
Additionally, according to the theory of molecular mimicry, gluten proteins are structurally similar to, and may “mimic” parts of the thyroid gland, so the body may mistakenly attack the thyroid gland, contributing to symptoms seen in Hashimoto’s.
Various tests can be done to determine if one has either celiac disease or non-celiac gluten sensitivity (gluten intolerance). However, the condition may not always show up on these tests, as some celiac tests may show false negatives. Some individuals do not learn of their gluten sensitivity until they remove gluten from their diets for a trial period, or take an IgG blood test. (You can learn more about testing for gluten sensitivity here.)
As such, I highly recommend that every person with an autoimmune thyroid condition remove gluten from their diet, to see if doing so helps to resolve symptoms.
Action steps for this root cause:
- Take an IgG test to check for gluten sensitivity, OR
- Remove gluten from your diet for 2-3 weeks, to see if symptoms improve and/or resolve.
- Note: If celiac disease is suspected, consult your healthcare practitioner and request a celiac test.
If gluten was the sole root cause that had triggered your autoimmune disease, you should see a complete remission of thyroid antibodies, and thyroid function may even return to normal, within three to six months! If not, you may need to dig deeper…
Root Cause #2: Food Sensitivities
In addition to gluten sensitivity, individuals with Hashimoto’s may also be reactive to multiple other foods and their proteins, such as those found in gluten-free grains (e.g. rice, quinoa, corn). Some experts, like Dr. William Davis, author of Wheat Belly, claim that human beings did not evolve to eat “grasses” like wheat, rice, or corn. As such, these difficult-to-digest foods are more likely to become food sensitivities for us.
Some of us with Hashimoto’s may also react to dairy, soy, eggs, nuts, seeds, nightshades, and many other foods. In my survey of over 2000 individuals with Hashimoto’s, 58 percent of responders said they react to gluten, 45 percent said they react to dairy, and 28 percent reported reacting to soy.
Food sensitivities differ from allergies in that they activate separate branches of the immune system. While food allergies are generated by the IgE branch of the immune system, food sensitivities are generated by the IgG, IgA, and IgM branches, and reactions do not appear immediately.
An allergy to peanuts, for example, may result in an itchy rash, throat swelling, low blood pressure, shortness of breath, or other potentially life-threatening symptoms, within minutes of consuming the culprit food.
A food sensitivity reaction, on the other hand, may take a few hours to a few days to manifest, and may present through less common symptoms such as skin lesions or breakouts, fatigue, acid reflux, bloating, irritable bowel syndrome, palpitations, joint pain, anxiety, tingling, or headaches.
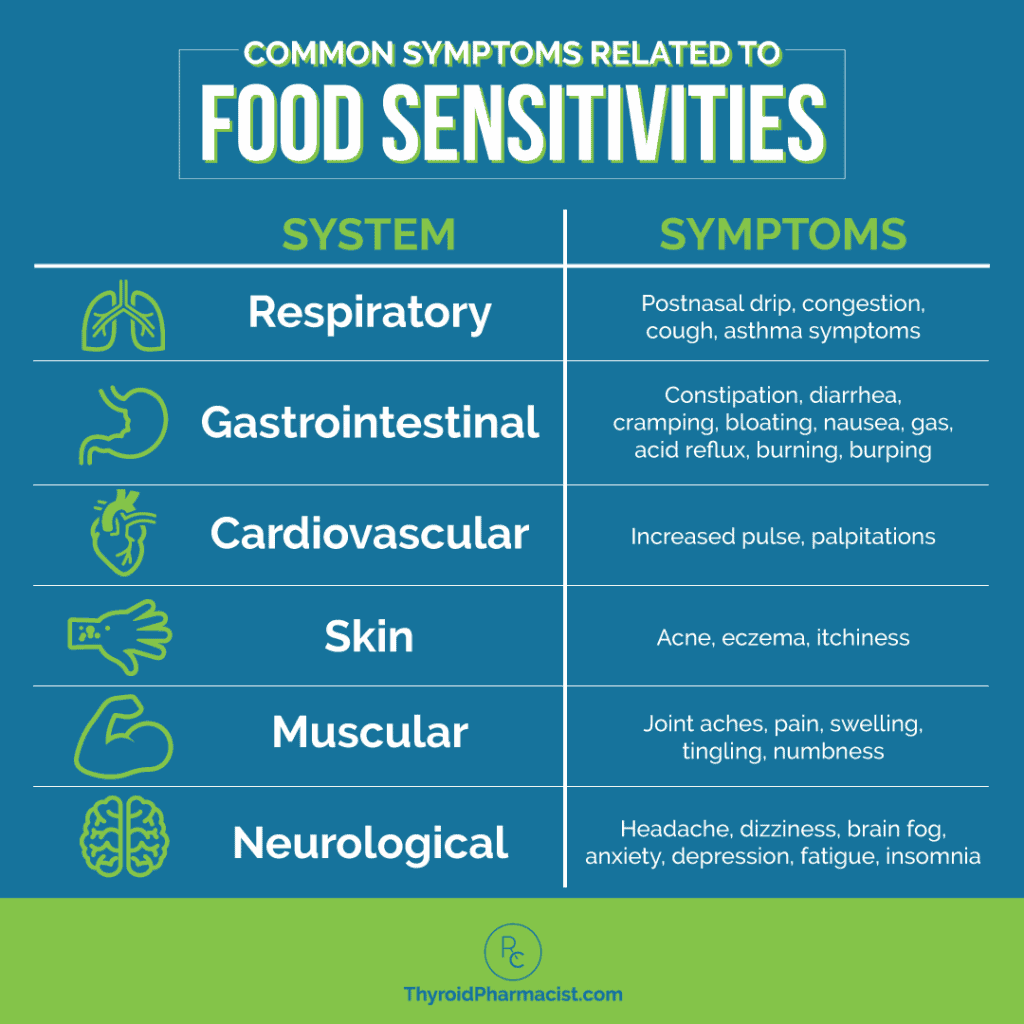
Food sensitivities may occur for a variety of reasons. One reason is the presence of leaky gut, as proteins from the aforementioned foods can enter the bloodstream via “leaky holes” within the gut. Other factors such as inflammation and stress, can also contribute to food sensitivities.
Thus, identifying and removing foods that one is sensitive to from their diet, can help reverse leaky gut. Often, an individual can reintroduce these foods once the gut is healed (with the exception of gluten).
Action steps for this root cause:
- Identify your personal food sensitivities to avoid. (MyMedLab offers two options to test for the most commonly eaten foods: the 184 Food Panel and the 96 Food Panel; alternately, consider doing an elimination diet.)
- Consider following a Paleo or Autoimmune Paleo (AIP) diet, and in some cases, a rotation diet, as these diets may be beneficial for supporting a healthy gut (they omit foods that individuals with Hashimoto’s are most commonly sensitive to, and tend to focus on nutrient-dense foods). I have a free 2-week AIP recipe plan that may be helpful, if you’re not sure where to start with the AIP diet. Additionally, working with a nutrition coach can be extremely helpful in this respect.
- Consider taking supplements that can help restore the gut lining, such as L-glutamine. (Learn more about such supplements in the next section of this article.)
- Take systemic enzymes such as Wobenzym, as they may prevent reactions to new foods, and reduce reactions to current foods.
Root Cause #3: Glutamine/Zinc Depletion
Zinc and glutamine are two substances (among others) that are required for rebuilding the intestinal lining. In times of stress, the body will pull these substances from our intestines and use them for other processes, such as the production of adrenal hormones.
In most cases, these substances become available to us through food, things go back to normal after the stressful time is over, and the gut lining is quickly rebuilt with new nutrients.
However, this becomes an issue for those under prolonged stress, those with low stomach acid (which is needed to extract zinc from proteins), and those that follow a diet low in animal protein (such as vegan and vegetarian diets), as glutamine is primarily found in animal protein (including eggs and dairy). High amounts of zinc are found in animal products such as oysters and red meats, though zinc can also be found in some plant sources such as various beans (which many people with Hashimoto’s are sensitive to).
Some individuals who once followed vegan/vegetarian diets and then decide to reintroduce animal proteins back into their diets, have been able to put their Hashimoto’s in remission. I believe this is because the glutamine and other ingredients allowed them to rebuild their gut lining.
As such, I recommend optimizing your glutamine and zinc levels via supplementation, if you are found to have suboptimal levels of zinc and glutamine.
You can test your zinc levels through a self-ordered ALP (alkaline phosphatase) test (low zinc levels are reflected through low ALP levels). Glutamine levels can be tested through the Great Plains Amino Acids Urine Test and the Great Plains Amino Acid Plasma Test, which analyze 40 different amino acids (including glutamine), as well as several markers of nutrients needed for amino acid functions.
Action steps for this root cause:
- Consider taking a glutamine supplement. Research has shown that supplementing up to 0.65 g per kilogram of body mass is well tolerated. I generally recommend 5 g per day as a good place to start, then working up to a target dose of 15 g per day (divided into three doses of 5 g each, at breakfast, lunch, and dinner), or as tolerated.
- Please note: I generally recommend taking glutamine for two to six months. However, some practitioners believe that high doses of glutamine can become excitotoxins and fuel cancer cells. If you have any symptoms that might suggest that it’s an excitotoxin, such as brain fog, nervousness, edginess, or light headedness, then I would stop taking it. As always, please discuss any new supplements with your practitioner before taking them, to ensure they are appropriate for you.
- Consider taking a zinc supplement (at a dose of no more than 30 mg/day) to reach optimal levels (reflected by ALP levels between 70 and 90 IU/L).
- Consume foods high in glutamine (like bone broths, gelatin, and well-cooked meats).
- Consider taking Betaine with Pepsin or digestive enzymes to extract zinc from food, if low stomach acid is an issue. (It is, in fact, common in those with Hashimoto’s. You can read more about low stomach acid here.)
- Consider following a nutrient-dense diet, such as the Paleo or AIP diet.
Root Cause #4: Parasites
You may think that parasites are only present in malnourished third world countries, but this is not the case. Depending on the sources, it has been estimated that 30-70 percent of Americans may be infected with parasites! Current detection methods miss many parasites, and few people ever get tested for them.
That said, parasitic infections are common triggers of Hashimoto’s.
Some common parasitic infections that I’ve found in many of my clients, include:
Symptoms may vary depending on the parasite, though some common symptoms include fatigue and GI disturbances (bloating, nausea, changes in bowel movements) — I recommend checking each linked to article for a deep dive into how each infection affects those with Hashimoto’s.
A parasite found in the intestines can cause a tremendous amount of damage and has the ability to cause intestinal permeability by creating holes in the intestinal wall. Due to this ability, parasites can also lead to the development of food sensitivities and autoimmune disease. If you are someone who developed your condition after a period of intense stress, I urge you to get tested, as stress makes us more susceptible to parasites.
Some people follow restrictive diets to help with the onset of food sensitivities often caused by parasites. Unfortunately, diets are a short-term fix. People with parasites have multiple food sensitivities that don’t go away no matter what they eat or don’t eat. A person may feel better initially after removing sensitizing foods, only to start feeling worse once new foods become reactive.
You can be on the perfect diet, and take loads of supplements, but if you have a parasite, it doesn’t matter; you will not be able to recover fully until the infection is eradicated.
There are many different types of parasites, including worms, amoebas, and protozoa. Different treatments work for different parasites. Thus, while general parasite cleanses can sometimes help, I prefer to figure out the specific type of parasite that you’re dealing with, through advanced testing (such as the GI-MAP, GI Effects, or Comprehensive Stool Analysis tests).
For parasites in those with autoimmune disease, I take the approach “guilty until proven innocent,” as I have seen many people with five to ten negative tests for parasites, finally come up positive on one of the above-mentioned tests.
If you do test positive for one or more parasites, I recommend working with a knowledgeable practitioner who can help guide you through protocols to eradicate them. You can also read more about my recommended protocols for parasites in my book, Hashimoto’s Protocol.
Many of them incorporate the use of the probiotic S. boulardii, which can promote a healthy gut flora, help prevent infections, and even support your body in clearing some infections (check out my article on S. boulardii for how to best take this supplement).
Action steps for this root cause:
- Test for parasites with one of the following tests: GI-MAP, GI Effects Comprehensive Profile, or Comprehensive Stool Analysis from Great Plains Laboratory (you can self-order them or order them through a functional medicine practitioner).
- Consider specific antiparasitic medications or herbal protocols (tailored to the parasite).
- Consider taking the probiotic S. boulardii.
Root Cause #5: Small Intestinal Bacterial Overgrowth (SIBO)
The small intestine is supposed to contain relatively minimal amounts of bacteria. However, in certain cases, an overgrowth of bacteria in the small bowel or small intestine, called small intestinal bacterial overgrowth (SIBO), can occur. A 2007 study found that 50 percent of people with hypothyroidism had SIBO.
This overgrowth can be caused by antibiotic overuse, low stomach acid, bowel motility issues, or a poor diet, among other factors. The small intestine is more vulnerable to overgrowths and imbalances of gut flora, as it has significantly less microbiota compared to the large intestine (making the environment less competitive).
SIBO can result in intestinal permeability, or leaky gut, as the body tries to get rid of the excess bacteria in the small intestine (and contributes to the holes being created in the intestinal wall).
SIBO is associated with symptoms such as acid reflux, belching, and bloating (those with SIBO will notice a flat stomach upon waking, which quickly bloats after a meal). Additionally, those with SIBO will most likely notice a flare up of these symptoms after eating fibrous foods, fermented foods, cruciferous veggies, and prebiotics/probiotics, which feed the bacteria overgrowth.
I have seen people with Hashimoto’s resolve symptoms like IBS, restless leg syndrome, low ferritin, and low B12 levels by treating SIBO; and in some cases, I’ve also seen thyroid antibodies reduced — and even completely go away — with SIBO treatment. Additionally, healing SIBO can in turn, help heal leaky gut.
Action steps for this root cause:
- Test for SIBO – I recommend the Small Intestinal Bacterial Overgrowth 3-Hr Lactulose-Genova Kit.
- Consider taking antibiotics and/or antimicrobial herbs to eradicate SIBO (I often recommend oil of oregano, Candibactin-BR and Allicillin) — check out my SIBO article for an overview of the different protocols that can be helpful.
- Consider following a healing diet such as the Elemental diet, Specific Carbohydrate diet, Low FODMAP diet, or GAPS diet, as such diets can promote gut healing and are often recommended for those with SIBO.
Root Cause #6: Fungal Infections
The fungus (and yeast) Candida has been implicated in autoimmune disease and food sensitivities. Factors such as following a high-carbohydrate diet, having high estrogen levels (as seen in pregnancy or in those with estrogen dominance), experiencing high levels of stress, and taking medications that alter the pH of the intestines and/or gut microbiome, can make an individual more susceptible to a Candida infection.
This pathogenic yeast can contribute to the development of intestinal permeability, or leaky gut, by using its hyphae (branching) form to weaken and penetrate the intestinal barrier, leaving holes in the intestinal wall.
Once these holes are created, this fungal pathogen is able to release several endo- (internal) and exo- (external) toxic byproducts into the bloodstream. The release of byproducts not only worsens leaky gut, but also contributes to autoimmunity.
Common symptoms of a Candida infection include:
- Food sensitivities
- Fatigue
- Bloating, especially from carbohydrate-rich foods
- Gas
- Belching
- Diarrhea or constipation
If these symptoms resonate with you, I recommend reading my article on Candida for an in-depth explanation of how it affects Hashimoto’s, and specific recommendations (including guidelines on the supplements/diets mentioned below) to address it. I also invite you to read holistic nutritionist Liz Schau’s Hashimoto’s remission story after overcoming Candida.
Action steps for this root cause:
- Test for overgrowth of Candida in the bowels — the GI-MAP test is a great option.
- Follow an anti-Candida diet such as the Body Ecology diet.
- Take anti-fungal supplements and/or medications (such as oil of oregano, S. boulardii, and the other supplements outlined in my article on Candida), to address the infection.
The Takeaway
Intestinal permeability, or leaky gut, can be caused by several different root causes — I’ve highlighted six in this article. From my own personal journey and my experience with helping thousands of others with Hashimoto’s, I’ve found that digging at and addressing the root cause(s) of one’s leaky gut, can be the most effective long-term solution for gut health. (Remember that without a leaky gut, the three-legged stool of autoimmunity can’t stand, and autoimmune conditions can go into remission!)
Going through the list of root cause factors, testing for confirmation, and incorporating the solutions mentioned above, can improve and eliminate intestinal permeability. (If some interventions require supplements, be sure to discuss them with your practitioner prior to taking them, to ensure they are appropriate for you.)
Even though it may take some time, I encourage you to “dig at it!” to find your root cause.
It’s not always the same for each person, which is why I wrote my book, Hashimoto’s: The Root Cause, to help you figure that out! I cover each of the above-mentioned root causes in great detail, including how each one impacts Hashimoto’s, and give guidance on how to find your specific root cause (or set of root causes). This book also provides the opportunity to learn about additional root cause factors that may be at play behind your thyroid condition (there are too many to list in one article!).
For a self-explanatory way to kickstart your gut health journey, I also encourage you to download my free gut guide eBook. The guide offers a variety of solutions for the gut issues mentioned in this article.
I hope this helps, and I wish you all the best on your healing journey!
You can also download a free Thyroid Diet Guide, 10 thyroid-friendly recipes, and the Nutrient Depletions and Digestion chapter of my Root Cause book for free. You will also receive occasional updates about new research, resources, giveaways and helpful information.
For future updates, make sure to also follow us on Facebook and Instagram!
References
- Sategna-Guidetti C, Volta U, Ciacci C et al. Prevalence of thyroid disorders in untreated adult celiac disease patients and effect of gluten withdrawal: an Italian multicenter study. The American Journal of Gastroenterology. 2001;96(3):751-757. doi:10.1111/j.1572-0241.2001.03617.x.
- Velentino R, Savastano S, Maglio M, Paparo F, Ferrara F, Dorato M,et.al. Markers of Potential Coeliac disease in patients with Hashimoto’s Thyroiditis. European Journal of Endocrinology. 2002;146(4):479-483.
- Lerner A, Jeremias P, Matthias T. Gut-thyroid axis and celiac disease. Endocrine Connections. 2017;6(4):R52-R58. doi:10.1530/EC-17-0021.
- Gleeson M. Dosing and efficacy of glutamine supplementation in human exercise and sport training. J Nutr. 2008;138(10):2045S-2049S. doi:10.1093/jn/138.10.2045S
- Vojdani A, Tarash I. Cross-Reaction between Gliadin and Different Food and Tissue Antigens. Food and Nutrition Sciences. 2013;4(1):20-32. doi:10.4236/fns.2013.41005.
- Cardoso-Silva D, Delbue D, Itzlinger A, et al. Intestinal Barrier Function in Gluten-Related Disorders. Nutrients. 2019;11(10):2325. Published 2019 Oct 1. doi:10.3390/nu11102325
- Rezaie A, Pimentel M, Rao S. How to Test and Treat Small Intestinal Bacterial Overgrowth: an Evidence-Based Approach. Current Gastroenterology Reports. 2016;18(2). doi:10.1007/s11894-015-0482-9.
- Hofer U. Fungal Pathogenesis: Candida’s toxic relationship with its host. Nat Rev Microbiol. 2016;14(5):268. doi:10.1038/nrmicro.2016.53
- Birdsall T. Gastrointestinal Candidiasis: Fact or Fiction? Altern Med Rev J Clin Ther. 1997;2:346-354.
- Iwata K. Toxins produced by Candida albicans. Contrib Microbiol Immunol. 1977;4:77-85.
Note: Originally published in February 2015, this article has been revised and updated for accuracy and thoroughness.


 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Hi Isabella,
Thank you so much for sharing your knowledge with us.
I wonder if one was diagnosed with multiple parasites, like h.pylori, Sibo and Candida, should all of them be tackled at the same time or separately?
I imagine that taking all the supplement at once would not be beneficial.
Thank you X
Anna – you are very welcome! ❤️ The way that you want to address infections is by starting with the highest infection in your body first. H. pylori is typically found in the stomach (it can also be in the upper part of the small intestine), so that’s going to be the first infection you want to treat. A lot of times, when you treat H. pylori, the SIBO will go away as well. Next would be the parasite. If, after the H.pylori and parasite protocols you still have SIBO, you would treat it at this time. The yeast would be addressed last, if needed. Sometimes when you use the parasite protocol along with the SIBO protocols, the yeast issue is taken care of as well. With the exception of discussing proper thyroid medication dosing, the majority of my website and my book focuses on balancing the immune system. The info I present is based on my own research and journey for overcoming my autoimmune thyroid condition. I discuss protocols for all of these in my book and on my website. Here are some resources that I hope you will find helpful.
Hashimoto’s Root Cause
https://amzn.to/2XXCqcQ
Hashimoto’s Protocol
https://amzn.to/3cJ89T4
Hello Dr. Izabella, recently I went to a biological dentist and she did a special x-ray called a cone beam CT SCAN that shows I have two infections where I had root canals done in which she advises I have these back teeth extracted and she will clean out the infections with ozone and also remove mercury on my other teeth… it will be a long extensive expensive treatment but I am wondering if this could be my root cause of Hashimoto’s with infection going through my bloodstream.. I was on the fence on what to do but I don’t want infection going to my brain or heart… So do you think this could be my root cause?? Thanks for your advice. Sincerely, Deborah
Deborah – thank you for sharing your journey. I’m so sorry you are going through all of this. Yes, infection in the mouth, even a minor one that disrupts the oral microbiome, can potentially trigger autoimmune disease. Here is an article I hope you find helpful:
https://bruno-michael-wentz.dev01.rmkr.net/articles/dental-triggers-hashimotos/
Hey Doc,
I’ve read the root cause and wanted to ask a few questions on food. Would things like Buffalo Sauce be considered ok for gut health or does that fall in the category of “peppers”?
I’ve also ready your post about Stevia. If you have it sparingly with things when its in a desert or something similar would you say it’s ok for gut health? Or is this something you think is best to stay away from entirely?
Also, in phase 1 of root cause should I be avoiding eggs and non-dairy cheese etc?
Thanks 🙂
Matt – thank you for reaching out! ❤️ If you are following an AIP diet or sensitive to the ingredients then I would not recommend the buffalo sauce. As for the stevia again it depends on whether you are sensitive to it. Feel free to email my team at info@thyroidpharmacist.com with any other questions about my protocols and they will be happy to help!
Hi Izabella,
I live in Canada. I did the GI Map and I have been found with various infections. H pylori, Akkermansia muciniphila, Firmicutes, Bacillus spp., Staphylococcus aureus and protoza parasites ( Blastocystis hominis, Dientamoeba fragilis and Endolimax nana).
My Nd gave me The FullMoon Kit for over a year. It didn’t work . Every unwanted guest is still present. Now, I am taking antibiotics ( Apo-Metronidazole). Do you think this is the right approach?
Laetitia – thank you for following and sharing your journey. Infections and parasits can be stubborn and hard to get rid of. Generally speaking, my clients have found success in treating gut infections through the use of antibiotics, herbal support, or a combination of both. I’m so glad you have a practitioner to work with you. I do recommend discussing your options and keeping them up to date on how your are doing. Please keep me posted on your progress. ❤️
You don’t mention viral infections being a root cause in this article? If we suspect herpes simplex as being the route cause how should this be treated? I can’t find any advice on this particular issue. Thanks
H – thank you for following. Here is an article that I hope you find helpful: https://bruno-michael-wentz.dev01.rmkr.net/articles/viruses-may-trigger-hashimotos/