In my clinical experience, I’ve seen many cases of thyroid problems go undiagnosed (or misdiagnosed) because most doctors don’t perform a comprehensive thyroid panel.
I spent almost a decade undiagnosed because I only had one marker tested. My thyroid condition was missed completely, leading me to deal with needless “mystery” symptoms like chronic fatigue, depression, anxiety, and many others, for far too long!
I still have a copy of my lab results from 2008, before I was diagnosed with Hashimoto’s. At that time, I was desperately searching for a reason behind my exhaustion, hair loss, anxiety, and digestive issues. According to this lab report, my TSH was at 4.5 μIU/mL, yet there was a note written from the doctor declaring: “Your thyroid function is normal, no need to do anything.” Perhaps a TSH of 4.5 μIU/mL would have been normal for a 95-year-old woman, but I was 25 and sleeping 12+ hours a night to feel rested!
Of course, even as a pharmacist, I didn’t think to question the doctor — and most people don’t.
If you suspect that you may have a thyroid condition, or know someone who does, this article will go over all of the most helpful tests that can help you identify a thyroid condition.
This article will also teach you how to understand your labs so that you can advocate for proper treatment for yourself.
In this article, I’ll go over:
- The top thyroid tests that I recommend
- How to interpret your results
- Understanding reference ranges
- How often you should test your thyroid
- How to use lab results for medication adjustments
Thyroid Tests 101
Testing thyroid hormone levels is the first step in diagnosing a thyroid disorder and determining the appropriate course of treatment. However, I’ve found that many doctors don’t test for Hashimoto’s, despite having their patients present with symptoms of thyroid disease.
Due to conventional guidelines, most primary care doctors simply test one’s TSH (thyroid stimulating hormone) and T4 levels (the amount of the T4 thyroid hormone circulating in your blood), to screen for hypothyroidism. However, these tests are not always interpreted correctly, don’t differentiate between non-autoimmune thyroid issues and Hashimoto’s, and often miss the subtle fluctuations of thyroid hormones and elevated thyroid antibodies that occur in the early stages of Hashimoto’s and hypothyroidism. These stages are often symptomatic and may last a decade before the TSH or T4 levels are flagged as abnormal. Sadly, from personal experience, conversations with other functional practitioners, and hearing reports from clients, I’ve often seen that people with these early stages of Hashimoto’s are told, “Your thyroid tests are normal, there’s nothing wrong with you”, even when they are clearly exhibiting symptoms of thyroid dysfunction that could be clearly confirmed by additional testing.
For this reason, it’s important to have a full thyroid panel done, which includes not only TSH and T4, but also T3, along with the two most common Hashimoto’s antibodies, TPO and TG antibodies. (When they are elevated, they indicate an autoimmune process within the thyroid gland. Their level can indicate the strength of the autoimmune attack against the thyroid gland and can help with predicting a timeline of full thyroid destruction.)
Additionally, an ultrasound test can help to diagnose Hashimoto’s, as well as reveal what’s happening with your thyroid and see if there are any nodules present.
I’ll go into detail about why each thyroid test is important below, but I do recommend getting a full thyroid panel done so that you have all of the information necessary to take charge of your health. [1]
Please be sure to review the bottom section of this article about lifestyle, medications, and supplements, as there are several other factors which may affect your thyroid test results.
Please note: The recommendations in this article are based on my clinical experience, and follow current research and recommendations by practitioners in functional medicine. They may not be recognized by doctors who are not familiar with functional medicine.
How to Order Your Lab Tests
If your doctor is ordering thyroid labs for you, be sure to request a copy so that you can see them for yourself and ensure that they are interpreted correctly.
Additionally, I have included self-order options for most of the labs discussed, in case your current doctor won’t order the labs for you.
The self-order options are discounted panels that I set up with Ulta Labs and can be ordered almost anywhere in the U.S. (direct access testing is prohibited by law in New York, New Jersey, and Rhode Island). You will receive a lab order that can be taken to your local lab, and the results will be sent to you electronically.
You can order each individual test that I recommend below, or you can order the entire discounted panel (TSH, free T3, free T4, TPO antibodies, TG antibodies) here.
In many cases, you can self-order the labs and then send the receipts for reimbursement to your insurance. (Please check with your insurance FIRST to ensure that they will accept this and what their procedure is.)
Now, let’s take a look at each thyroid test and what they mean for your thyroid health.
1. The Thyroid Screening Test
The thyroid stimulating hormone, or TSH test, is used as a screening test for thyroid disease, as well as a test for monitoring the correct dose of medication needed for an individual.
This is an important test that I recommend getting every time you check your thyroid function.
TSH is a pituitary hormone that responds to low/high amounts of circulating thyroid hormone. If you’re new to thyroid lab testing, it may seem counterintuitive, but an elevated TSH means that you do not have enough thyroid hormone on board and that you are hypothyroid. This is because the TSH hormone senses low thyroid levels and is released when there is a lack of it, in an effort to signal the body to make more.
In advanced cases of Hashimoto’s and primary hypothyroidism, this lab test will be elevated. In the case of Graves’ disease and hyperthyroidism, TSH levels will be low. People with Hashimoto’s and mild or central hypothyroidism may have a “normal” reading on this test.
If you’ve been a thyroid patient for a while, you’re probably thinking to yourself, “Well, of course, doesn’t everyone know that?” — and I have to warn you… I’ve unfortunately seen physicians who have mistakenly thought that a low TSH meant one had an underactive thyroid, and a high TSH, an overactive thyroid — putting their patients in really dangerous situations by under- or overmedicating them!
In recent years, The National Academy of Clinical Biochemists indicated that 95 percent of individuals without thyroid disease have TSH concentrations below 2.5 μIU/mL, and a new normal reference range was defined by the American College of Clinical Endocrinologists to be between 0.3 and 3.0 μIU/mL. [2]
However, in my experience of reviewing the labs of thyroid patients from around the world, many labs have not adjusted that range in the reports they provide to physicians, and some even have ranges as lax as 0.2 to 8.0 μIU/mL. Thus, conventional medicine practitioners will likely follow the standard reference range for TSH to determine if a person has hypothyroidism — in some cases, they may even follow a more lax range if the lab they are using hasn’t updated their levels, or if the practitioner is not familiar with newer guidelines.
In any case, physicians who follow “standard” reference ranges may end up telling their patients that their thyroid is normal, when in fact, they have a thyroid condition! And many physicians may miss the patients who are showing an elevated TSH. This is one reason why patients should always ask their physicians for a copy of any lab results.
Some practitioners consider a range of between 0.35 mIU/mL and 4.50 mIU/mL as normal, while others suggest using a range of between 0.5 mIU/mL and 2.50 mIU/mL as normal. [3] However, many of my colleagues in the functional medicine community, as well as myself, have further defined that normal reference ranges should be between 1 and 2 μIU/mL for a healthy adult not taking thyroid medications. And thus, for optimal health, a person with hypothyroidism should be properly treated until their TSH reflects that of a healthy person with optimal function. 🙂
When I was in Poland to find distributors for the Polish version of my first book back in 2014, I happened to visit one of my relatives who was wearing a heavy winter coat on a warm spring day. In speaking with her, I was able to tell that she was experiencing a great number of thyroid symptoms, and she confided that her doctor had said her thyroid was normal. I looked at her labs, and sure enough, her TSH was around 5 μIU/mL, and she was never tested for antibodies nor offered a thyroid ultrasound. (I often share that at the time of my diagnosis, I was living in Southern California and sleeping under two blankets, and was walking around with a TSH of 4.5 μIU/mL – and guess what, I survived living in Colorado for six years when my thyroid was optimized. :-))
I have found that I, as well as many other thyroid patients, feel best when my TSH is between 0.5 and 2 μIU/mL (for elderly clients, up to 2.5 μIU/mL). Some integrative professionals will go as far as to say that people should have a TSH of right around 1 μIU/mL or below 1 μIU/mL, to feel their best.
That said, the TSH test is not the only test that should be used to diagnose Hashimoto’s since, in the early stages, one’s TSH level may fluctuate or remain within the normal limits.
Most conventional practitioners will stop further thyroid testing when they determine the TSH is “normal” (that is, within the outdated, old school “normal” reference range).
This is why, even if you’ve been told your thyroid is normal, and even if your TSH is between 0.5 and 2 μIU/mL (the range I recommend), you need to test your free T4, free T3, and especially thyroid antibodies (TPO antibodies and TG antibodies), to truly determine if you have a thyroid condition.
Recommended test: TSH
Optimal reference range: Between 0.5 and 2 μIU/mL
How often you should test: Every four to six weeks when starting a new medication, then every six months if symptoms are stable.
Things to consider before testing: I recommend testing your TSH early in the morning, and delaying your thyroid hormones until after taking the test, to ensure accurate results, especially if you are taking T3-containing medications. Taking your medications before the test can suppress your TSH and make it look like you are overmedicated when you are not. Additionally, the supplement biotin, commonly used for hair loss, can also suppress TSH levels, making it look like you are overmedicated, or like you are hyperthyroid. The American Thyroid Association recommends that patients stop taking biotin for at least two days before a TSH test.
2. Thyroid Hormone Level Tests
There are four main thyroid hormones that have been identified: T1, T2, T3, and T4.
T4 (thyroxine) and T3 (triiodothyronine) are the two main thyroid hormones. T4 is known as prohormone and is 300 percent less biologically active than T3. T3 is the main biologically active thyroid hormone and gives us beautiful hair, replenishes our energy, and runs our metabolism. [4]
You may have put together that most of the commonly prescribed thyroid medications like Synthroid and levothyroxine, only contain T4 (thyroxine), and thus they need to be converted to the active T3 form in the body.
On paper, the T4 to T3 conversion happens just fine, but in the real world, in real human bodies, we may not always convert T4 to T3.
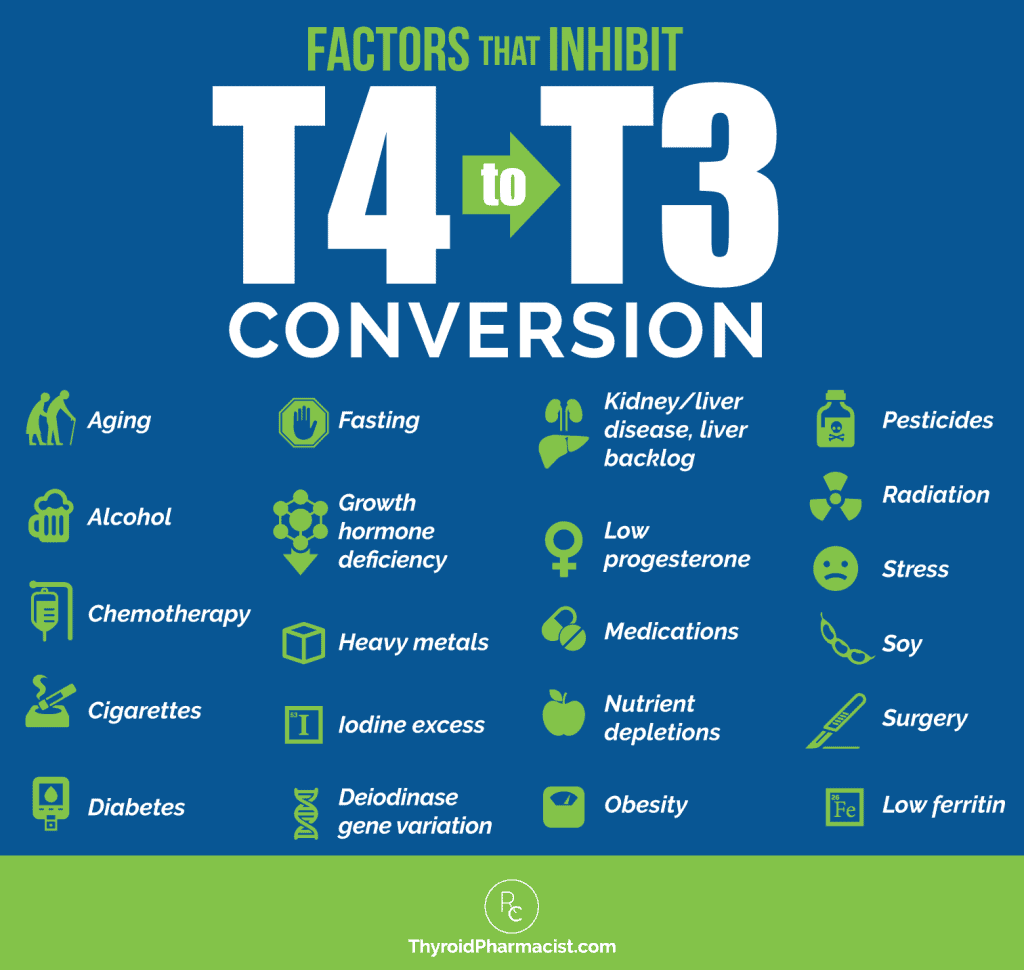
We can reveal our T4 to T3 ratios and measure the hormone that is available to do its job in the body, by testing our free T4 and free T3 levels.
Free T3 and Free T4 tests measure the levels of active thyroid hormone circulating in the body. (When these levels are low, but your TSH is in the normal range, this may lead your physician to suspect a rare type of hypothyroidism known as central hypothyroidism. I’m working on an article on this topic, so stay tuned!)
Some clinicians may only test for T4, but T3 is also important to test, as some individuals may not be converting T4 to the active T3 properly. Thus, people may have a normal T4, but a low T3 level.
How Do You Know If You Are Converting Correctly?
Take a look at your free T3 and free T4 levels. Both should be in the optimal ranges noted below, which have been determined by functional medicine guidelines and my clinical experience. If the T4 is optimal, but the T3 is below the optimal range, you know that your body is not making enough T3 hormone from the T4.
In rare cases, we may see low T4 levels and high T3. This is typically seen in pregnancy, when someone has an increased requirement for T4 and may benefit from adding extra T4 for the baby’s development. You can learn more about this in my article on pregnancy and Hashimoto’s. Outside of pregnancy, it’s not common to see low T4 and high T3.
Recommended test: Free T3 and Free T4
Optimal Free T4 reference range: 15 to 23 pmol/L
Optimal Free T3 reference range: 5 to 7 pmol/L
How often you should test: I recommend testing every four to six weeks when starting a new medication, every two to three months if tracking the impact of lifestyle changes, and then every six to 12 months once symptoms are stable.
Things to consider before testing: I recommend testing your free T3 and free T4 early in the morning, and delaying your thyroid hormones until after taking the test to ensure accurate results, especially if you are taking T3-containing medications. Taking your medications before the test can result in a falsely elevated T3 (and sometimes T4), making it look like you are overmedicated when you are not. Additionally, the supplement biotin, commonly used for hair loss, can also falsely increase both T4 and T3 levels, making it look like you are overmedicated, or like you are hyperthyroid. The American Thyroid Association recommends patients stop taking biotin at least two days before a T4 and T3 test.
3. Thyroid Antibodies
There are various types of antibodies against the thyroid gland that can be detected in thyroid disease. The presence of thyroid antibodies indicates that the thyroid gland has been recognized as a foreign invader by the immune system and that the thyroid gland is under attack.
In Hashimoto’s, triggers contribute to the body developing something called “a lack of self-tolerance.” This is when the body is no longer able to recognize its own tissue as part of itself, but instead starts viewing its tissue as a foreign invader. It is no longer “tolerant” of itself, and this is what leads to an autoimmune condition. When the body begins this breakdown of its immune tolerance, we’re initially going to see the presence of elevated thyroid antibodies.
In Hashimoto’s, about 80 to 95 percent of patients have thyroid antibodies. [5] Thyroid antibodies are going to be the first indication of a thyroid problem in many cases. They can be elevated for 5, 10, sometimes even 15 years, before a change in TSH is even detected. Having elevated thyroid antibodies, even in the presence of a “normal” TSH, means that it’s only a matter of time before your thyroid becomes destroyed to the point that it can no longer produce a sufficient amount of hormones.
Some clinicians will say that once you have thyroid antibodies, you will always have thyroid antibodies, so the actual number doesn’t matter, as the antibodies can randomly fluctuate. I respectfully disagree.
I believe that antibodies can fluctuate in response to triggers (some as common as stress), and in my exhaustive experience, they can be an incredibly helpful marker for tracking disease progression.
The most common antibodies in Hashimoto’s are thyroid peroxidase antibodies (TPO antibodies) and thyroglobulin antibodies (TG antibodies). Most people with Hashimoto’s will have an elevation of one or both of these antibodies. TPO antibodies are the most common and have been reported in 5 to 38 percent of the population, depending on the study! [6]
Thyroid antibodies are often elevated for decades before a change in TSH is seen in Hashimoto’s.
People with Graves’ disease and thyroid cancer may also have an elevation in thyroid antibodies, including TPO and TG. However, the most common antibodies found in Graves’ disease are TSH receptor antibodies, including thyroid-stimulating immunoglobulin (TSI) — this marker is elevated in over 90 percent of people with Graves’ disease. [7] TSH receptor binding antibody (TRAb), also known as TSH-binding inhibiting immunoglobulin or TBII, is elevated in over 50 percent of people with Graves’ disease. [8] (You can check for Graves’ related antibodies here.)
Thyroid antibodies can be used for diagnostic purposes and monitored to track remission. As I mentioned, thyroid antibodies indicate an active destruction going on against your thyroid. This destruction often comes with a lot of symptoms that may cause, or be misdiagnosed as depression, panic attacks, anxiety, miscarriage/infertility, carpal tunnel, hair loss, weight gain, fatigue/laziness, and, of course, the most disempowering diagnosis of them all… hypochondria.
Hypochondria is a diagnosis I take great offense to because it ignores the patient’s intuition that there is something wrong. It often leads to shame, disempowerment, helplessness, and the destruction of trust we have in our own mind and body connection, as well as in the healthcare model and of ever getting well.
The good news is that in many cases, when you have elevated antibodies and a normal TSH, you can not only reverse all of your symptoms, but you can also prevent damage to your thyroid gland using a root cause approach.
I found out I had thyroid antibodies in the 2000 IU/mL range, one year before doing a thyroid function retest, when my thyroid function deteriorated to the point where my doctor thought I would benefit from medications. Unfortunately, the doctor that initially ran the antibody test told me not to worry about them, and that there was nothing I could do anyway. I am often saddened that I trusted another person with my health and didn’t do additional research on my own. I was also highly symptomatic at that time, likely due to the elevated TPO antibodies. I had new onset panic attacks, social anxiety, hair loss, digestive issues, and fatigue — common early symptoms of elevated thyroid antibodies.
As a 25-year-old newlywed who had just moved to a new city, I was crippled by my health. Instead of focusing on being a newlywed, making my wedding albums, and meeting new friends, I felt like I was falling apart. The crazy thing is, I am now in my late 30s, with a busy little boy and a business, and I feel 10 times more energetic than I did in my 20s! I no longer grieve the decade I lost to undiagnosed Hashimoto’s, but this is why I’m so passionate about advocating for you to get the proper tests, and for you to understand your tests!
Thyroid antibodies may be elevated for many years before a change in TSH is seen, and finding antibodies early can often prevent damage to the thyroid, as well as help with preventing the need for long-term medications.
As mentioned earlier, thyroid antibodies can also be used as a marker to monitor disease progression and remission. While any elevation of thyroid antibodies can indicate Hashimoto’s (and some may have seronegative Hashimoto’s with thyroid antibodies not elevated at all), I like to monitor thyroid antibodies in clients.
While not all clinicians will agree to the following ranges, based on research and my clinical experience, here are the numbers I keep in mind:
- Thyroid antibodies above 500 IU/mL are considered a very aggressive case of Hashimoto’s
- Antibodies under 100 IU/mL indicate remission, or a less aggressive case
- Antibodies under 35 IU/mL mean you no longer test for Hashimoto’s according to conventional medicine standards
- Antibodies under 2 IU/mL are optimal (scientists believe that there may be some antibodies present as part of a normal repair process)
I recommend a lot of strategies to make the condition less aggressive and to put it into remission, in my article on reducing thyroid antibodies, as well as in my books Hashimoto’s: The Root Cause and Hashimoto’s Protocol. Be sure to check them out to learn how to lower your antibody levels.
Recommended tests: TPO, TG for Hashimoto’s (and TSI, TBII for Graves’). Please note that some TPO tests will only test up to 900 IU/mL, so if you know you have high levels of antibodies and would like a test that gives you more accurate numbers, be sure to check with the lab on their parameters before ordering. The TPO Antibody Endpoint test from Quest will give you TPO values beyond the 900 IU/mL limit, all the way up to 10,000 IU/mL, while the Thyroid Peroxidase Antibodies (TPO) version does not go above 900 IU/mL.
Optimal TPO reference range: <2 IU/mL
Optimal TG reference range: <2 IU/mL
Optimal TSI reference range: < 0.55 IU/L
Optimal TBII reference range: 16 to 100 percent inhibition of TSH binding
How often you should test: I recommend monitoring thyroid antibodies every 60-90 days to see if the changes you’re making in your lifestyle are helping you. A reduction in these antibodies, especially when accompanied by a reduction in symptoms, is a good indication that your condition is improving and that you are on the right path with your healing interventions.
4. The Thyroid Ultrasound
Some individuals may have thyroid disease but may not have detectable alterations in their blood work. In fact, research suggests that 10 to 50 percent of people with Hashimoto’s may not test positive for antibodies. [9] In these cases, a person might have a less aggressive version of Hashimoto’s known as antibody negative or seronegative Hashimoto’s.
In these cases, a thyroid ultrasound can be used to find physical changes in the thyroid gland that point to Hashimoto’s.
A thyroid ultrasound will help you and your physician determine whether you have changes consistent with Hashimoto’s (such as a rubbery thyroid, shrunken thyroid, enlarged thyroid, or abnormal growths in the thyroid that are present). Some growths may indicate an autoimmune process, others may indicate benign nodules, and others may signal cancerous nodules.
I can’t locate the reference at the moment, but I have learned that some 10 percent of people diagnosed with Hashimoto’s are diagnosed using an ultrasound, and I recommend that everyone with Hashimoto’s or thyroid disease get at least one ultrasound in their lifetime, especially women of childbearing age. If thyroid nodules are found, then I recommend having an annual ultrasound. (Be sure to read my comprehensive article on shrinking thyroid nodules if you happen to have them.)
A thyroid ultrasound is a very simple, non-intrusive test that only takes about 10 minutes. It uses sound waves to image the thyroid. A lubricant jelly is placed on the skin and a small hand-held transducer is passed over the thyroid. The ultrasound will show any change in gland size and texture. Clinicians can find changes in thyroid size (shrunken or enlarged), tissue density and texture (rubbery), as well as nodules (abnormal growths), which are all characteristic changes found with Hashimoto’s. Growths can also be a signal for cancerous nodules. If there is a concern with that, the next step would be to have a nodule biopsy, and you can read more about that in my article on thyroid cancer.
Recommended tests: Thyroid ultrasound ordered by your physician (I am not aware of self-order options at this time)
How often you should test: I recommend at least one ultrasound for every person, especially women of childbearing age.
5. The Reverse T3 Test
The reverse T3 (rT3) test measures how much of the active free T3 hormone is able to bind at thyroid receptors. RT3 is produced in stressful situations and binds to thyroid receptors, but turns them off instead of activating them. (Stress is a common cause of low T4 to T3 conversion. Under stressful situations, T4 gets converted to reverse T3 instead of to T3. Reverse T3 is an inactive molecule related to T3, but without any physiological activity.) [10]
The rT3 test is sometimes used to identify cases of poor T4 to T3 conversion, as well as thyroid symptoms that are due to adrenal stress, instead of thyroid malfunction or autoimmunity.
However, in most cases, this test doesn’t change my other recommendations, so I consider this an optional test. (I prefer the adrenal saliva test to determine the proper treatment for adrenal stress. An adrenal saliva test gives us the advantage of knowing how to address the reason one is producing too much reverse T3.)
The free T4/free T3 test is more useful for me to determine if a person is properly converting thyroid hormones. In cases where a lot of reverse T3 is produced, adding a thyroid medication that contains T3 ensures that the right hormone is getting to the right receptors.
This test will likely not be used by conventional doctors, but many integrative doctors love the reverse T3 test, and it may be a useful test to monitor your improvement. So if you think that this test (or others listed here that are not part of a conventional assessment) might be useful for you, consult with a functional practitioner in your area. (I have a handy database of functional practitioners here on my website — but please note that I do not endorse or make representation as to the qualifications or business practices of any healthcare provider.)
When assessing your rT3 results, it is important to watch for trends of your levels going up. This usually indicates your body is reacting to a stressful situation. Your body produces rT3 to give it a break and to prevent you from becoming hyperthyroid. This is an evolutionary adaptation to slow your metabolism in times of famine (for more information on this, take a look at my Safety Theory). High rT3 due to stress has a snowball effect on hypothyroid symptoms. The adaptation by the body producing rT3 is not useful in our high-demand society when we must work and take care of our children, spouse, parents, etc.
Recommended tests: Reverse T3 (rT3)
Optimal rT3 reference range: Between 11 and 18 ng/dl
How often you should test: Every six months, if recommended by your integrative physician.
6. Your Symptoms
Last but not least, your symptoms should serve as an important thyroid test. Be sure to listen to your body — only you know its subtle messages!
Our symptoms offer vital clues as to what is going on inside our bodies, and these symptoms can shift as our thyroid hormone levels change.
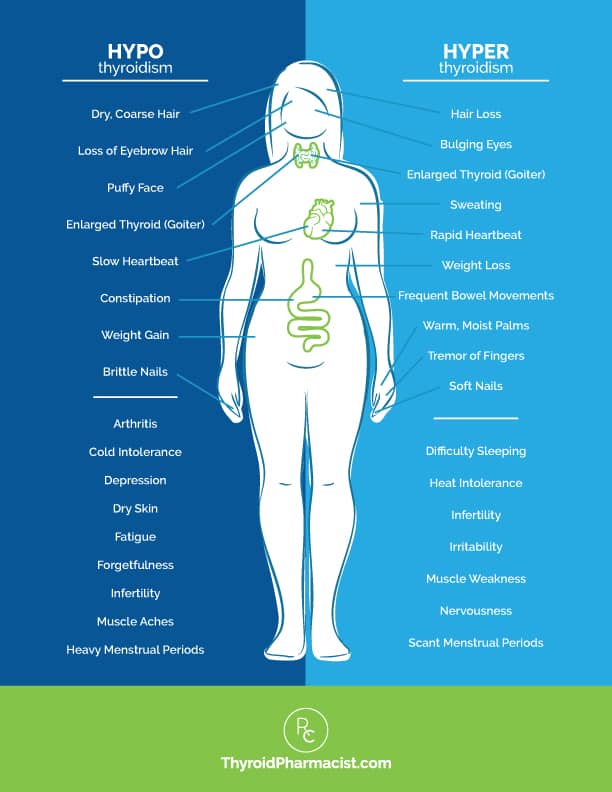
Do you have any symptoms of hypothyroidism, or deficiency of thyroid hormone, such as:
- Slower metabolism leading to weight gain
- Forgetfulness
- Feeling cold or cold intolerance
- Depression
- Fatigue
- Dry skin
- Constipation
- Loss of ambition
- Dry, coarse hair
- Muscle cramps
- Stiffness
- Joint pain
- A loss of the outer third eyebrow
- Heavy menstrual periods
- Infertility
- Muscle aches
- Puffy face
- Slow heartbeat
- Brittle nails
- Arthritis
Or, do you have any symptoms of hyperthyroidism, or an overabundance of thyroid hormone, such as:
- Weight loss
- Palpitations
- Anxiety
- Eye-bulging
- Tremors
- Irritability
- Infrequent menstrual periods
- Fatigue
- Heat intolerance
- Increased appetite
- Hair loss
- Enlarged thyroid gland
- Sweating
- Frequent bowel movements
- Infertility
- Soft nails
- Warm, moist palms
- Finger tremors
- Insomnia
- Muscle weakness
- Nervousness
In addition to many of the symptoms we frequently see associated with hyper- and hypothyroidism, Hashimoto’s commonly presents with:
- Anxiety
- Depression
- Weight gain
- Mood swings
- Fatigue
- Brain fog
- Cold hands and feet
- Gastrointestinal issues
- Food sensitivities
Some of these symptoms may be directly related to insufficient thyroid hormone. Others may be due to related issues (i.e. gut infections), which I have seen in many people with Hashimoto’s. That’s why it’s important to identify the root causes of YOUR Hashimoto’s, so you can take the first steps toward healing!
Recommended tests: Create a health timeline and use a notebook or chart to keep track of your symptoms.
Reference Range: Score the severity of your symptoms from 1-10, and aim to steadily lower your score by uncovering and addressing your root causes.
How often you should test: I recommend assessing your symptoms on a weekly basis until you feel you have eliminated them.
Interpreting Your Labs
Once you have your labs, what do you do with them? What do they mean?
I frequently get messages from readers asking me to comment on their thyroid labs. Of course, I can’t provide medical advice through the internet without doing a personalized comprehensive case review (this is for your own safety as well as due to professional liability laws), so I wanted to write this little guide for you all to empower you to understand your own labs.
Please note: This evaluation is based on optimal functional medicine ranges and my clinical experience, and may not be recognized by doctors who are not familiar with functional medicine.
Optimal Reference Ranges
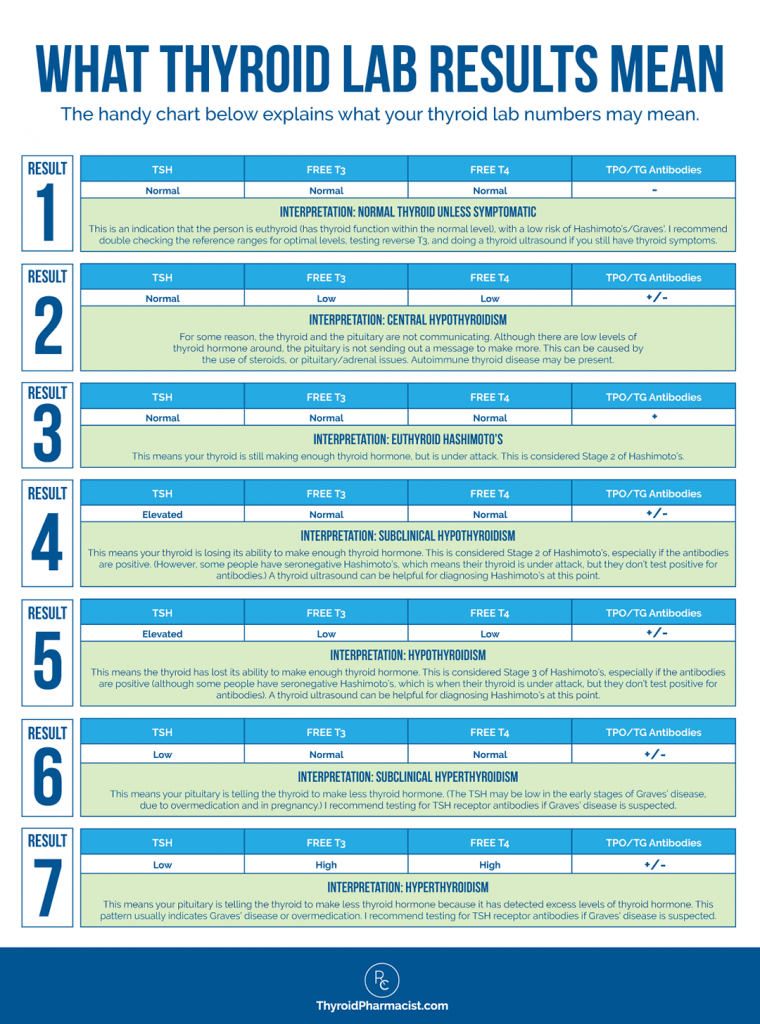
When I look at my client’s labs, I’m focusing on optimal reference ranges. Here’s a handy reference chart I created for Hashimoto’s, based on recommendations from my training with the Institute of Functional Medicine:
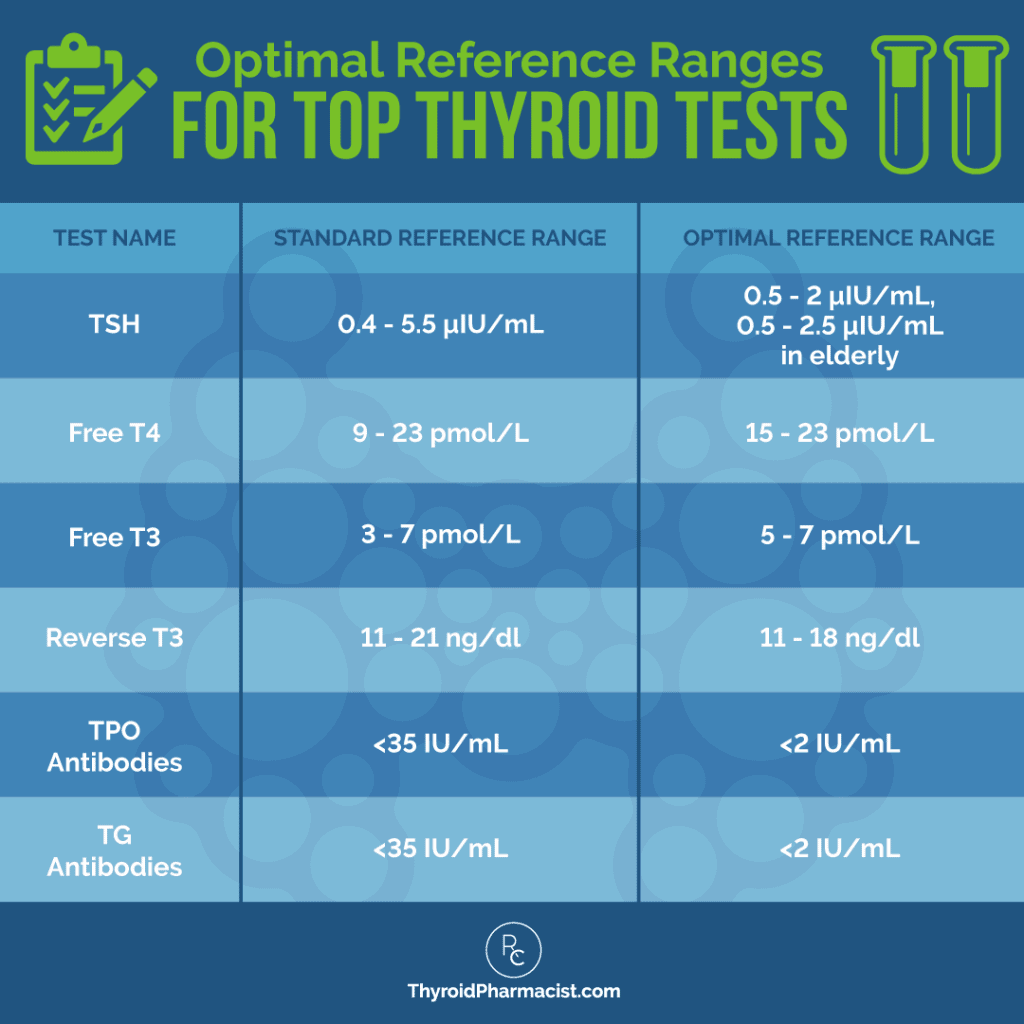
The handy chart below explains what the thyroid lab numbers mean:
Your optimal thyroid numbers are going to be different from your mother’s optimal thyroid numbers, which are going to be different from your neighbor’s optimal thyroid numbers, so it’s important for you to track your thyroid symptoms while tracking your numbers, to determine your “personal best.”
Understanding Thyroid Labs for Medication Prescriptions and Adjustments
Thyroid labs, especially TSH, free T3, and free T4, are critical for determining if you need to start, increase, or reduce the dose of your thyroid hormone medications, as well as if you’re on the right thyroid medications.
Some physicians who prescribe thyroid medications will not prescribe a medication unless the TSH is above 10 μIU/mL, and will be satisfied when a person who is taking thyroid meds has a TSH under 10 μIU/mL. I think this is the reason why many people continue to have fatigue, cold intolerance, difficulty with weight loss, and hair loss — despite taking thyroid medications.
When the TSH is between 2.5 μIU/mL and 10 μIU/mL, and/or when T3 and T4 are within normal limits, this is known as subclinical hypothyroidism. This means that the thyroid is still able to make enough thyroid hormone, but not without sacrifice. At this point, our thyroid is working overtime, leading to many of the common symptoms of hypothyroidism.
The thyroid is constantly getting a signal to make more and more hormone, and your body is likely running out of nutrients (like selenium) to make more hormone. This results in additional inflammation to the thyroid, attracting more antibodies and fueling the autoimmune process. While some may stay in a subclinical state indefinitely, researchers suggest that 2-28 percent of patients with subclinical hypothyroidism progress to overt hypothyroidism, depending on age, gender, and the presence of anti-thyroid antibodies. [11] In my experience, on average, five percent of people with subclinical hypothyroidism may progress to overt hypothyroidism each year due to this and the THEA Score. (Please review my article on thyroid antibodies for more information on this.)
What About Thyroid Medications for Subclinical Hypothyroidism?
Starting thyroid medication in subclinical hypothyroidism is considered controversial by endocrine groups. Exceptions are made for women who are contemplating pregnancy and for those who have overt hypothyroid symptoms. Guidelines clearly state that in order to avoid pregnancy complications and impaired development of offspring, women with subclinical hypothyroidism need to be treated with thyroid hormones. [12]
At this stage, many patients may also opt to “wait and see” and may forgo thyroid medications in an effort to “do it naturally.” I know that I was one of those people, and I waited six months to get on medications after my diagnosis, but knowing what I know now, I am in favor of starting medications for subclinical hypothyroidism.
Why?
Korzeniowska and colleagues at the Medical University of Gdansk found that treating children with subclinical hypothyroidism with thyroid hormones, resulted in a decrease of inflammation. [13] This means that the medications gave their thyroids a rest and resulted in a slowing down of the autoimmune attack, manifested by lower levels of thyroid antibodies.
Additionally, in my clinical experience, most patients with subclinical hypothyroidism report feeling much better when they start on thyroid hormones.
Personally, when I was first diagnosed with subclinical hypothyroidism, I didn’t want to take medications because I felt like it would be giving up, and that I should figure things out naturally.
At that point, I started weekly acupuncture sessions, eating Brazil nuts, and using all kinds of magic hair potions to try to keep my hair loss at bay (I was still a young butterfly then).
I wanted to believe that these interventions were keeping me from getting worse… until my husband and I took a red-eye flight from Los Angeles to visit friends on the East Coast in the winter. The lack of sleep combined with the cold weather put me in a hypothyroid flare.
I spent the entire weekend shivering, tearful, and anxious, and was very embarrassed about how much I inconvenienced our friends.
After I flew back to California, I spent a few days getting nourishment from the sun and made an appointment to start medications. I felt much better when I did, and thus I’m no longer a proponent of being a martyr for a senseless cause. Part of loving yourself is knowing when you need help.
If I could do it over, I would have, of course, gone gluten, dairy, and soy free for three months as soon as I had found out I had Hashimoto’s AND started medications. If a three-month trial of diet didn’t result in significant improvement, I would have started digging for my root cause.
After all, when my TSH was at 4.5 μIU/mL, I was sleeping for 12+ hours, and at 3 μIU/mL, my hair began to tangle. I didn’t realize how hypothyroid I was until I was appropriately treated. A little change in the dosage of thyroid medication can make a huge difference.
What About Those Already on Thyroid Medications?
If you’re already on thyroid meds, but still have symptoms, it is possible you may need to up your dosage so that your labs fall within the optimal range, to help you feel better.
Please take a look at my article on TSH for a letter that you can take to your physician if he/she is not familiar with the current optimal reference range. As I mentioned earlier, I personally feel best with a TSH a bit under 1 μIU/mL, but you may need some trial and error to find your personal best TSH.
Once you establish a dose of medication that’s working for you — and as long as your symptoms don’t change (look out for anxiety and palpitations as potential signs of an overdose, and fatigue and pain as potential signs of an underdose) — you can test your thyroid hormones every six months.
You may want to read about the different hormone preparations in my article A Pharmacist’s Review of Medications for Hashimoto’s and Hypothyroidism.
Other Considerations for Hormone Testing
There are some other important factors you should know about that can affect your thyroid test results and hormone levels.
Thyroid medications are goldilocks hormones, which means they need to be used in just the right dose — and there are risk factors of being overmedicated.
I recommend testing thyroid hormone levels every six to 12 weeks while using complementary therapies, including root cause medicine, diet, or supplements that may optimize your thyroid function, improve the absorption of thyroid medications, and/or reduce your requirement for thyroid medications (you know, all the stuff I recommend on my website!), as well as when incorporating new lifestyle changes, to ensure your thyroid medication dosage is optimized — or sooner, if you are showing any of the above-mentioned symptoms.
Symptoms of overmedication include, but are not limited to: rapid or irregular heartbeat, nervousness, irritability or mood swings, muscle weakness or tremors, diarrhea, menstrual irregularities, hair loss, weight loss, insomnia, chest pain, and excessive sweating. Do not start, change, increase, decrease or discontinue your medications without consulting with your physician.
Supplements and Medications That May Interfere With Thyroid Test Results
It’s important to note that there are various medications and supplements that can impact your thyroid test results.
While some supplements can result in false readings of thyroid levels (such as the biotin I listed above), others reflect a true change in thyroid levels — this change may be an actual improvement or worsening of levels depending on the supplement. The change may be long-lasting even after the substance is removed, while others may produce changes in thyroid levels that are temporary and will resolve once the substance is removed (i.e. drug interactions).
- Substances That Cause Long Lasting Improvement in Thyroid Function: I’ve found that aloe vera, cordyceps, vitamin A, ashwagandha, and myo-inositol could lower/normalize TSH in some cases, meaning that people will need less medication.
- Substances That Cause Long Lasting Worsening of Thyroid Function: Medications like lithium, amiodarone, and high-dose iodine can cause thyroid damage, resulting in a greater need for thyroid hormones. [14] Please read this article for more information on medications that can be toxic for your thyroid, and this article about how to get accurate lab tests for more information on supplements and medications that can affect thyroid lab results.
- Temporary Alterations in Thyroid Function/Drug Interactions: Drug interactions, which occur between thyroid hormones and various medications, supplements, and foods, can lead to actual changes in thyroid hormone levels that are reversible once the interacting medication is stopped. Some examples include: calcium supplements, coffee, and OTC PPIs such as omeprazole. These tend to be most relevant if you take thyroid tablets within a few hours of taking these (the exception would be a gelcap formulation like Tirosint, which you can learn more about here). Talk to your doctor or pharmacist if you’re concerned about interactions with your thyroid medication.
To summarize, there are medications that interfere with thyroid lab results by actually interfering with thyroid hormone function — this means they cause real alterations in thyroid hormone levels. Some of these alterations are clinically significant and may require a dose adjustment of your thyroid medications when taking the two medications concurrently.
Please be sure to report to your practitioner any and all medications and supplements you are currently taking, as well as any changes in supplement or medication regimes.
Monitoring Your Thyroid Hormones When Making Lifestyle Changes
Whenever you start a lifestyle or complementary intervention to address Hashimoto’s, I encourage you to work with your doctor to monitor your thyroid symptoms, thyroid hormones, and thyroid antibodies. This is a great idea for any lifestyle intervention, but a must for lifestyle changes that could impact your TSH, especially if you are already taking thyroid medications.
Lifestyle changes and introducing new supplements could lower/normalize TSH in some cases, thus potentially reducing your requirement (or need) for thyroid meds. So as you move forward, please look out for the following symptoms of being overmedicated: rapid or irregular heartbeat, nervousness, irritability or mood swings, muscle weakness or tremors, diarrhea, heat intolerance, menstrual irregularities, hair loss, weight loss, insomnia, chest pain, and/or excessive sweating.
I recommend testing thyroid hormone levels every six to 12 weeks while using complementary therapies, including root cause medicine, diet, or supplements, to ensure your thyroid medication dosage is optimized – or sooner, if you are showing any of the above symptoms. Thyroid medications are goldilocks hormones – they need to be used in just the right dose – and there are risk factors of being overmedicated.
Testing TSH, T4, T3, and the two most common Hashimoto’s antibodies, TPO and TG antibodies, is an important part of ensuring that the lifestyle changes you are making are both safe and helpful. 🙂
The Takeaway
It can be a little bit overwhelming to figure out where to start with testing, but I hope the information in this article has helped you understand which thyroid tests you need to ask for, and how to interpret and act on the results.
In summary:
- If you suspect that you may have Hashimoto’s or hypothyroidism, I recommend that you get the following tests for diagnostic purposes: TSH/free T3/free T4 and TPO/TG antibodies, thyroid ultrasound.
- If you suspect that you may have Graves’ disease or hyperthyroidism, I recommend that you get the following tests for diagnostic purposes: TSH/free T3/free T4, a thyroid ultrasound, TSI and TBII antibodies.
- If you are monitoring your response to thyroid hormones or thyroid-suppressing medications, I recommend checking your TSH, free T3 and free T4 levels every four to six weeks.
- If you are monitoring for remission, I recommend testing TPO antibodies and TG antibodies for Hashimoto’s, or TSH receptor antibodies for Graves’, every 90 days.
I hope you found this article helpful in navigating your thyroid tests. As always, my goal is to empower you to take charge of your own thyroid health and feel your very best!
Was this article helpful? Did you have an “aha” moment? Do you have additional questions for me about labs?
I’d love to give you my 100-page eBook, Optimizing Thyroid Medications (a $19.99 value), for free! This eBook does a deep dive into the various thyroid medication options available, how to take them properly, and how to work with your doctor to get the right medication and the right dose.
P.S. You can also download a free Thyroid Diet Guide, 10 thyroid-friendly recipes, and the Nutrient Depletions and Digestion chapter of my first book, for free. You will also receive occasional updates about new research, resources, giveaways and helpful information.
To stay connected, please follow my Facebook, Instagram, TikTok, and Pinterest pages, where you can ask questions and interact with the thyroid community!
References
[1] Garber JR, Cobin RH, Gharib H, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association [published correction appears in Endocr Pract. 2013 Jan-Feb;19(1):175]. Endocr Pract. 2012;18(6):988-1028. doi:10.4158/EP12280.GL
[2] NH, Papaleontiou M. Biochemical Testing in Thyroid Disorders. Endocrinol Metab Clin North Am. 2017;46(3):631-648. doi:10.1016/j.ecl.2017.04.002
[3] Sheehan MT. Biochemical Testing of the Thyroid: TSH is the Best and, Oftentimes, Only Test Needed – A Review for Primary Care. Clin Med Res. 2016;14(2):83-92. doi:10.3121/cmr.2016.1309; Wartofsky L, Dickey RA. The evidence for a narrower thyrotropin reference range is compelling. J Clin Endocrinol Metab. 2005;90(9):5483-5488. doi:10.1210/jc.2005-0455
[4] Shahid MA, Ashraf MA, Sharma S. Physiology, Thyroid Hormone. In: StatPearls. Treasure Island (FL): StatPearls Publishing; May 8, 2022.
[5] Fröhlich E, Wahl R. Thyroid Autoimmunity: Role of Anti-thyroid Antibodies in Thyroid and Extra-Thyroidal Diseases. Front Immunol. 2017;8:521. Published 2017 May 9. doi:10.3389/fimmu.2017.00521
[6] Amouzegar A, Gharibzadeh S, Kazemian E, Mehran L, Tohidi M, Azizi F. The Prevalence, Incidence and Natural Course of Positive Antithyroperoxidase Antibodies in a Population-Based Study: Tehran Thyroid Study. PLoS One. 2017;12(1):e0169283. Published 2017 Jan 4. doi:10.1371/journal.pone.0169283; Prummel MF, Wiersinga WM. Thyroid peroxidase autoantibodies in euthyroid subjects. Best Pract Res Clin Endocrinol Metab. 2005;19:1-15.
[7] Ochi Y, Inui T, Kouki T, Yamashiro K, Hachiya T, Kajita Y. Thyroid stimulating immunoglobulin (TSI) in Graves’ disease. Endocr J. 1998;45(6):701-708. doi:10.1507/endocrj.45.701
[8] Bell L, Hunter AL, Kyriacou A, Mukherjee A, Syed AA. Clinical diagnosis of Graves’ or non-Graves’ hyperthyroidism compared to TSH receptor antibody test. Endocr Connect. 2018;7(4):504-510. doi:10.1530/EC-18-0082; Barbesino G, Tomer Y. Clinical Utility of TSH Receptor Antibodies. Journ. Clin. Endoc. & Metab. 2013;98(6):2247-2255. doi:10.1210/jc.2012-4309.
[9] Staii A, Mirocha S, Todorova-Koteva K, Glinberg S, Jaume JC. Hashimoto thyroiditis is more frequent than expected when diagnosed by cytology which uncovers a pre-clinical state. Thyroid Res. 2010;3(1):11. Published 2010 Dec 20. doi:10.1186/1756-6614-3-11
[10] Helmreich DL, Tylee D. Thyroid hormone regulation by stress and behavioral differences in adult male rats. Horm Behav. 2011;60(3):284-291. doi:10.1016/j.yhbeh.2011.06.003
[11] Lee, J and Chung, WY. Subclinical Hypothyroidism; Natural History, Long-Term Clinical Effects and Treatment. In Current Topics in Hypothyroidism with Focus on Development. Ed. Eliška Potluková. 2013.
[12] Lazarus J, Brown RS, Daumerie C, Hubalewska-Dydejczyk A, Negro R, Vaidya B. 2014 European thyroid association guidelines for the management of subclinical hypothyroidism in pregnancy and in children. Eur Thyroid J. 2014;3(2):76-94. doi:10.1159/000362597
[13] Korzeniowska K, Jarosz-Chobot P, Szypowska A, et al. L-thyroxine stabilizes autoimmune inflammatory process in euthyroid nongoitrous children with Hashimoto’s thyroiditis and type 1 diabetes mellitus. J Clin Res Pediatr Endocrinol. 2013;5(4):240-244. doi:10.4274/Jcrpe.1136
[14] Haugen BR. Drugs that suppress TSH or cause central hypothyroidism. Best Pract Res Clin Endocrinol Metab. 2009;23(6):793-800. doi:10.1016/j.beem.2009.08.003; American Thyroid Association. Clinical Thyroidology for the Public. Clin Biochem. Epub 2018 Jul 20. PMID: 30036510. Accessed July 7, 2022. https://www.thyroid.org/patient-thyroid-information/ct-for-patients/december-2018/vol-11-issue-12-p-3-4/
Note: Originally published in February 2015, this article has been revised and updated for accuracy and thoroughness.


 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Please comment on iodine testing. We are exposed to halogens that displace iodine, also increasing the risk for thyroid disease as well as enlarged prostate among other things.
Susan – thank you for reaching out. ❤️ Here is an article I wrote that I hope you find helpful:
IODINE AND HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/iodine-hashimotos/
Dear Isabelle, have you done a great job with this blog? It is fantastic! I am a vet myself and have discovered my Hashimoto thanks to your online presence.
Now my team and I try to do a better job in thyroid therapies with our small patients.
You are a great game changer! Thank you so much!
Jacqueline, thank you so much I’m so glad you and your team are finding my research helpful when treating your small patients as well! I hope you will keep me posted on this! ❤️
I’m a retired surgeon, who had total thyroidectomy way back in 2002 for cancer. Been monitored yearly by my endocrinologist and frequently have to adjust the dosage. I’ve been reading tour book and on-line and truely enjoyed your passion on research. Wish I can contribute to what you are doing. Continue your good work.
DR. Juan, thank you so much! I’m so happy to hear you are enjoying my research! I would love to hear more about your experiences. Feel free to email my team at info@thyroidpharmacist.com and they will be happy to share with me! ❤️
This is such a useful article. Thank you so much. When using the chart of different stages to determine your potential stage of thyroid disease, do you use the standard reference ranges or the optimal reference ranges?
Jo – thank you for following! You would want to use the optimal reference ranges. ❤️
This is an amazing wealth of knowledge and experience. We, your patients and followers, can’t thank you enough. God will bless you for your gooddoings – you bring health to those who need it and those who want to be educated and enlightened. So noble, so generous. Be well and healthy. dear Dr. Wentz. We adore you…
Respectfully and with admiration.
Helen Litinsky
Helen, awe… you are so sweet! Thank you so much for your support! ❤️
Hi Dr. Wentz, I have been tracking my blood pressure and pulse and wanted to know if increased blood pressure, edema is a result of hyper- or hypo-thyroidism or Levothyroxin. I being treated 3+ years by a telemedicine homeopathic MD and symptoms, and semiannual TSH are all over the place with symptoms that seem to be hyperthyroid at times. I have a health record since Jan. 2020. I need better monitoring which is why I accessed this blog. Thanks for caring.
Mary – thank you for reaching out. <3 I'm so sorry you are struggling with all of this. It's hard to say without a comprehensive health assessment. I recommend that you discuss this further with your practitioner. People with Hashimoto’s may experience BOTH hypothyroid and hyperthyroid symptoms because as the thyroid cells are destroyed, stored hormones are released into the circulation causing a toxic level of thyroid hormone in the body, also known as thyrotoxicosis or Hashitoxicosis. Eventually, the stored thyroid may become depleted and due to thyroid cell damage, the person is no longer able to produce enough hormones. At this time, hypothyroidism develops. ❤️ Check out this article for more info:
https://bruno-michael-wentz.dev01.rmkr.net/articles/need-know-thyroid-disease/
I get terrible headaches, my eyes look like they are sinking, circles under my eyes, heart palpitations, gut issues, terruble fatigue, muscle soreness, joint pain and soreness in piece of thyroid leftover after thyroidectomy. My doctor lowered my dosage from 88 mg unithroid to half every other day and 15 mg of armour thyroid. I feel worse. I am at my wits end.
Marie – I am sorry to hear that you are are experiencing this. Sometimes it takes time to find a medication that is perfect for you. ❤️ You may benefit from switching your medication under the advice of your practitioner to see if you can find a medication that you can tolerate better. Taking your medication with selenium or lemon water may also help you to absorb it better. Here is an article you might find helpfule:
A Pharmacists Review of Medications
https://bruno-michael-wentz.dev01.rmkr.net/articles/medications-for-hashimotos-and-hypothyroidism/
My TSH is 5.45
Bounded T4: 7.62
Bounded T3: 130.5
What this report depicts?What should I do next??
Zeeshan – thank you for following. Thank you for reaching out! There are a lot of moving pieces and various triggers with thyroid disease, but there are also many actionable steps we can take to feel better! If you are just getting started on your healing journey, here are a few resources that may help:
ABOUT HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/about-hashimotos/
THE MANY FACES OF HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/the-many-faces-of-hashimotos/
WHERE DO I START WITH HASHIMOTO’S?
https://bruno-michael-wentz.dev01.rmkr.net/articles/where-do-i-start-with-hashimotos/
HASHIMOTO’S SUCCESS STORIES
https://bruno-michael-wentz.dev01.rmkr.net/articles/hashimotos-success-stories/
Thank you Izabella. Very helpful.
However, you don’t seem to have mentioned Secondary Hypothyroidism. I have Hashimotos and my TSH level is always very low – 0.01mIU/L in the latest test, which was why I was not diagnosed for a long time, although I had all the symptoms of hypothyroidism. You only mention low TSH in terms of hyperthyroidism.
I used to be on Armour Thyroid but it became impossible to get in the UK, and horrendously expensive if you could get it. I have been on 125 mcm Levothyroxine for about 10 years now, which is not brilliant but just about keeps my T4 and T3 within range.
Perhaps you could write about TSH deficiency in terms of hypothyroidism, when the pituitary is not sending the message to make more thyroid hormone.
Many thanks.
Alison
Alison, thank you for following! <3 TSH is a pituitary hormone that responds to low/high amounts of circulating thyroid hormone. Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it's important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress. Here is an article you might find interesting:
MEDICATIONS FOR HASHIMOTO'S AND HYPOTHYROIDISM
https://bruno-michael-wentz.dev01.rmkr.net/articles/medications-for-hashimotos-and-hypothyroidism/
Hi,
Does it matter what time of day you get your blood drawn for thyroid tests? Does it matter if you are fasting? I just want to be sure that we get the most accurate results.
Thanks,
Connie
Connie – thank you for reaching out! It depends! If you are taking a T4 only medication, you can go ahead and take your medication in the morning before the test. T4 medication has a long half-life, and your levels will be stable regardless of when you take it. If you take a T3 medication on the other hand, or a combination of T3/T4, T3 has a shorter half-life so your blood work may not be reflected accurately. It will appear that you have more thyroid hormone on board than you do. Thus it may be helpful to delay your morning dose of a T3/T4 medication until after you do the test to see (try to schedule the test in the morning). Here is a resource you might find helpful:
OPTIMIZING MEDS
https://bruno-michael-wentz.dev01.rmkr.net/checkout/?product_id=4702
Oh wow
What a wonderful guide .
I will be straight onto my Dr this week and get these tests done .
All the symptoms I have been having are here .
Thank you for so much clarity .
Best wishes
Alison
Alison, thank you so much! <3 I hope you will keep me posted on your progress!
Hi! My TSH value is 0.020 and my T4 is 7.7
My doctor told me that my thyroid is supressed and decreased my medicine from 120mg of NP Thyroid to 90 mg. I don’t feel well at all and still have symptoms of joint pain, cold intolerance, brain fog, hair loss etc. Do you have any adive?
Thank you!
Deanne – thank you for reaching out. <3 I'm so sorry you are not feeling well. Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it's important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress. Every six weeks is usually a good schedule for testing your thyroid hormones. There is more information on this in the articles above. Here are some other articles you might find helpful as well:
BRAIN FOG AND HASHIMOTO'S
https://bruno-michael-wentz.dev01.rmkr.net/articles/brain-fog-hashimotos/
IS GLUTEN THE ROOT CAUSE OF YOUR THYROID CONDITION?
https://bruno-michael-wentz.dev01.rmkr.net/articles/gluten-root-cause-thyroid-condition/
10 MOST HELPFUL DIY INTERVENTIONS FOR HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/10-most-helpful-diy-interventions-for-hashimotosaccording-to-my-clients
THYROID AND COLD INTOLERANCE
https://bruno-michael-wentz.dev01.rmkr.net/articles/thyroid-and-cold-intolerance
Hi Thks for your articles , wanted to know I’ve had lower end free t3 and total t3 for over 6 years mostly hair shedding . Pain on back now but other labs are normal Endo say t3 doesn’t matter if they would add t3 they would put me on hyper since my tsh is on lower side 0.5-1.5 range. Any suggestions? Thks
Yessy – thank you so much for reaching out. <3 Some people with Hashimoto’s, may not be able to properly convert levothyroxine (T4), the active ingredient in Synthroid, to liothyronine (T3), the more metabolically active thyroid hormone, leading to unresolved thyroid symptoms, including fatigue, depression, weight gain and hair loss, despite being on medications. For more information on various thyroid medication options, here’s an article I wrote:
WHICH THYROID MEDICATION IS BEST?
http://bruno-michael-wentz.dev01.rmkr.net/articles/which-thyroid-medication-is-best/
TOP 11 THINGS YOU NEED TO KNOW ABOUT THYROID MEDICATIONS
http://bruno-michael-wentz.dev01.rmkr.net/articles/top-11-things-you-need-to-know-about-thyroid-medications/
Dr. Wentz,
You have been huge in my hashimotos recovery, thank you!! I come from a family where almost every woman on my maternal side has hashimotos and now even three of my cousins. For over two decades I had symptoms and no one treated me. For the first time I’m on thyroid medicine and finally feel like a normal 30 year old woman!! My 5 year old daughter just got diagnosed with type 1 diabetes which they say goes hand in hand with hashimotos. Unlike most type 1s she should have lost weight but instead she just gains weight like crazy. I pushed to have her thyroid panel done since I didn’t want her to live my same story. My questions is these ideal lab numbers you give in this article, are they for children too?? She has antibodies between 10-25 and a 2.08 tsh. Her pediatrician immediately disregarded anything…please I would love your advice!!
Klynne – thank you so mmuch for sharing! 💕 The same labs used to diagnose thyroid disease in adults can be used for children. However, the lab values and reference ranges to look for may differ. My research is based on adults so I cannot provide information for children/babies, I recommend consulting your doctor for pediatric thyroid testing. Here are the tests you need for diagnosis. You may need to request them.
¨ TSH
¨ TPO Antibodies
¨ Thyroglobulin Antibodies
¨ Free T4
¨ Free T3
¨ Reverse T3 (optional)
¨ Thyroid Ultrasound (optional)
Here is a research article which might help further:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://bruno-michael-wentz.dev01.rmkr.net/articles/top-6-thyroid-tests/
I do suggest that you work with a functional medicine doctor that is familiar in working with children. I hope this helps!
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://bruno-michael-wentz.dev01.rmkr.net/articles/functional-medicine-approach-to-the-thyroid
CLINICIAN DATABASE
https://bruno-michael-wentz.dev01.rmkr.net/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://www.functionalmedicine.org/practitioner_search.aspx?id=117
Dear Dr Wentz
Thank you for this article!!
I have been diagnosed Hashimoto with antibodies over 1000 both, for 10 years. Today my antibodies are really low (between 12 and 25), my doctor said that it doesn’t means anything. If you have any advice on it…
Tsh has been around 0,01 since a year
T4 around 15 and T3 is 7,7
Thank you so much!
What if your results have different units than the ones in the above? T4 is ug/dL, t3 is listed as a %. I’ve googled conversions but that is quite a bit confusing, do you have any cheat sheets or tips on how to compare when units are different (or seemingly different)?
Laney – thank you for reaching out. ❤️ Different labs will have different ranges, a good general guideline is to get your Free T4 in the top half of the range, your Free T3 in the top half to top quarter of the range and your TSH around 1.5 or below.
Dr. Wentz, first of all, I thank you from the very bottom of my heart for all your work. I have found a very young and compassionate GP who is asking my guidance on her labs and how they should be interpreted & I have printed this entire article, twice, but CANNOT seem to print the “WHAT THYROID LAB RESULTS MEAN” page clearly even with adjusting sizing and it is not legible. I am older and not super tech-savvy, any help for me to print this clearly for her as my appt is tomorrow morning.
Appreciate you-!!
Meggie, you are so very welcome! ❤️ I’m sorry you were not able to print the page and that I was not able to respond to you before your appt. If you are still interested please email my team at info@thyroidpharmacist.com and they will be happy to help you! I do hope you will keep me posted on your progress.
I just ran the Ultra Lab panel and the range numbers don’t seem to match those you listed. Do your functional medicine ideal measurements sync with those of Ultra Lab? Ultra Lab in Oregon runs their tests through Quest. When I signed in I noticed I could give you access to my test results, which I did.
Carol – thank you so much for reaching out. ❤️ Please email my team at info@thyroidpharmacist.com and they will be happy to help you with this.
This information is excellent! I have had severe symptoms for months. I have been tested for Covid-19, 3 times, mono, iron deficiency ect. My exhaustion is on another level, I’m always freezing, can’t lose weight, have heart palpitations , anxiety and depression that comes and goes. I’ve been put on anxiety medication and a beta blocker. Still struggled, finally a doctor suggested I have my thyroid checked. All normal rage except my TPO antibodies are at 39. I have my fist doctor’s appointment tomorrow to follow up since we received my labs back. This is all so new to me, it’s a bit overwhelming! I’m so glad I found this article! After doing some of my own research I received 6 chemotherapy treatments and 16 radiation treatments to my chest after being diagnosed with non-Hodgkin lymphoma a week before my 28th birthday. I had a 12.9 cm mass in my chest. I am predicting the chemotherapy and radiation damaged my thyroid and the residual effects are just now showing up 7 years later at age 35. I pray this is fixed soon so I can have my life back!
Emily – thank you so much for sharing! ❤️ I’m so sorry you are struggling with all of this. I understand how overwhelming it can be. Hashimoto’s is often a combination of food sensitivities, nutrient deficiencies, adrenal issues, gut issues as well as an impaired ability to get rid of toxins. Any of those things would prevent a person from getting better. Hashimoto’s is very much an individual condition. While there are root cause commonalities, each person will have their own or in some cases, more than one root cause. You will have to start with the simplest modifications, by removing triggers, followed by repairing the other broken systems to restore equilibrium, allowing the body to rebuild itself. You will need to dig down to why the immune system is imbalanced in the first place and this will tell you how you begin to finally feel better, reduce your thyroid antibodies and even take your condition into remission.
You will have to create your own health timeline. Look back at your overall history as far back as you can remember. Look for infections, periods of severe stress, the use of medications (especially antibiotics, antacids, and oral contraceptives), accidents, and exposure to toxins. These are events that may have contributed to Hashimoto’s. Once you do, you will know what types of changes you need to implement to make yourself feel better. If you need further support, please check out the list of lab tests inside the “Testing” chapter of my book, Hashimoto’s Root Cause. I also offer a 12-week program, Hashimoto’s Self Management Program. Here are some resources I hope you find helpful as well. ❤️
BUILDING YOUR OWN HEALTH TIMELINE
https://bruno-michael-wentz.dev01.rmkr.net/sample-health-timeline/
Hashimoto’s Self-Management Program
https://bruno-michael-wentz.dev01.rmkr.net/enroll-in-hashimotos-self-management/
ROOT CAUSE RESET
https://bruno-michael-wentz.dev01.rmkr.net/enroll-in-root-cause-reset/
Hello! I have had tsh of .293 twice 6/8 weeks apart blood tests. No antibodies & normal t3/t4. Main issue is dry feels like burnt skin on arms and thighs at times had burning tongue as well. Dr still suspects subclincal hyperthyroidism. What can do to rebalbce by tsh or any advice? About 3 months of this. Trying to lower stress/anxiety going to through divorce at the same time. 🤷♀️
Misty – thank you so much for sharing you journey. I’m so sorry you are struggling with all of this. ❤️ Here are some articles I hope you find helpful:
GRAVES AND HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/graves-vs-hashimotos/
10 FACTS ABOUT THYROID DISEASE
https://bruno-michael-wentz.dev01.rmkr.net/articles/need-know-thyroid-disease/
PAIN AND HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/pain-and-hashimotos
I was diagnosed 7 years ago with Hashimoto, I am working on getting it under control,. I asked my Doctor to run my tests again to see where I am at, she told me that there be no need to repeat TPO antibody levels as this is purely used as a diagnostic tool. Once present, they will remain, but vary.” Is this true?
Thanks!
Kim – thank you for reaching out. ❤️ About 95% of people with Hashimoto’s have elevated Thyroid Peroxidase Antibodies, while 80% will have elevated Thyroglobulin Antibodies. They can both be important in monitoring the autoimmune attack on the thyroid, and can both be used to monitor the effect of interventions. Some interventions will lower TPO antibodies more, while others will have a greater effect on TG antibodies. This can depend on the individual and their body’s response.
Here are some articles I think you might find helpful:
HASHIMOTO’S AND THYROID ANTIBODIES: PART 1
https://bruno-michael-wentz.dev01.rmkr.net/articles/hashimotos-and-thyroid-antibodies/
HASHIMOTO’S AND THYROID ANTIBODIES: PART 2
https://bruno-michael-wentz.dev01.rmkr.net/articles/part-2-mechanisms-reduce-thyroid-antibodies/
I had early menopause at 41 yrs old and diagnosed with Hashimoto’s at 43. At 51 dexa scan showed osteopenia. I am 56 now and T score is -2.4. I will be full blown osteoporosis this year at the rate I am going. I started bioidentical HRT 9 years ago(6years into menopause) but it is not preventing bone loss. Is my thyroid hormone(Armour) causing my bone loss and what should I do about it. I have started rebounding recently.
Thank you for any help you can give.
Tina – thank you for sharing. ❤️ Monitoring progression of osteporosis is a good idea. I have found that nutrient depletions are always a factor in Hashimoto’s and addressing these nutrient depletions can make a HUGE difference in symptoms. These are some of the most important nutrient deficiencies I’ve found for people with Hashimoto’s:
6 MOST IMPORTANT NUTRIENT DEFICIENCIES IN HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/6-important-nutrient-deficiencies-hashimotos/
NEW STUDIES ON MAGNESIUM AND THYROID HEALTH
https://bruno-michael-wentz.dev01.rmkr.net/articles/new-studies-on-magnesium-and-thyroid-health
Thanks for all this information! What does it mean when reverse t3 is low: 10 ng/dL and free t3 is .3 (3 pg/mL)?
Jackie – thank you for reaching out.❤️ Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it’s important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress. Every six weeks is usually a good schedule for testing your thyroid hormones. Here is a research article which might help further:
TOP 10 THYROID TESTS
https://bruno-michael-wentz.dev01.rmkr.net/articles/top-10-thyroid-tests/
Hi Dr. Wentz,
I truly appreciate your detailed and in depth articles. They are very helpful. I happen to be one of the small percentage of men who has Hashimotos. Something I learned new from this article prompts a question: I have been intermittent fasting (16-18 hours per day) for quite some time now. In general, do you recommend or not recommend fasting for those with Hashimotos? Thank you, Cal
Cal – thank you so much for following! ❤️ While fasting can be beneficial in many cases, some caution is required for people with Hashimoto’s due to our blood sugar issues. Blood sugar imbalances are a big contributor to Hashimoto’s. Balancing blood sugar levels should be one of the priorities for anyone who is hoping to overcome autoimmune thyroiditis and adrenal fatigue. Balancing my blood sugar made a big difference for me, helping with my anxiety levels and reducing my thyroid antibodies. I hope this article helps shed some light on the matter:
BLOOD SUGAR IMBALANCES AND HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/blood-sugar-imbalances-and-hashimotos
It took some time before I realized that I had a hypothyroid problem. My grandmother had hypothyroidism, and unfortunately, I think that she had a bad change of medicine at one point and changed from NDT to T4 only. After that her memory began to deteriorate.
I didn’t get diagnosed till I had bad symptoms about 13 years after my daughter was born, but looking back I noticed possible symptoms like fatigue, forgetfulness, and even when I was 10 and ¾ years old I went through puberty. I grew very fast when I was young and when I hit puberty I stopped growing and everyone else passed me by in height. Until I had a daughter at 27, I seemed to be ok, but then I started the symptoms of fatigue, extreme hunger and forgetfulness. After about 13 years I was tested for hypothyroidism as my symptoms got really worse, and my TSH was just inside the standard range, so I would be considered normal. Fortunately, my doc thought I had a problem, but had to do many other tests to determine I did not have sleep problems, and other issues that doctors would otherwise think were the real issue. I started out on T4, but still had lots of leg pain, and could not walk more than 2 blocks without limping. So walking was not a good exercise for me to lose weight. I had access to a friend who was a doctor from Russia who served at Chernobyl who recommended trying NDT, and my doctor agreed to try this. The symptom got better, and then my pharmacist suggested adding extra T4 to the meds since NDT did not the right ratio as humans. This was a really good suggestion and I felt a lot better. Some years later, after I moved, I still didn’t feel really good, so when talking to a new pharmacist, he suggested that he could combine some T3 and a larger ratio of T4 in a time release capsule that would more precisely mimic human thyroid production. This has turned out to be a really good solution for me and I think is a very good solution for other hypothyroidism patients as well.
Do you think I may have had some hypothyroidism for most of my life, but didn’t get bad until after my pregnancy? That’s what I was thinking might have happened. I always try to find doctors now that have more insight into the real causes of my problem, and will do the right tests to diagnose my issues.
Joan – thank you so much for sharing your journey. ❤️It is possible. Pregnancy can also often be a trigger for developing Hashimoto’s or for an autoimmune flare – iron deficiency and immune shift, as well as potentially the baby’s thyroid cells that circulate in the body, may be a trigger. You might find this article interesting.
https://bruno-michael-wentz.dev01.rmkr.net/articles/estrogen-dominance-as-a-hashimotos-trigger/
Thanks so much for sharing your knowledge and wisdom with us!
I lost my thyroid to radiation 20 years ago due to Graves. I have been on Armour for the past 5 years and doing pretty well. My new PA is concerned that my TSH is .004 and keeps lowering my medication, but my Free T3 is now 3.0 and falling…and both my energy and mood are negatively affected from the reduced dosage of Armour. I suggested we try adding some liothyronine to the lower dosage of Armour. Any insights on how to best improve a .004 TSH? Thank you!
Caryn – thank you for reaching out. ❤️ In the case of autoimmune thyroid disease, removing the thyroid with a thyroidectomy eliminates thyroid antibodies, as there is nothing left to attack. However, life is not always roses with a thyroidectomy, as it does not remove the autoimmunity. If you’ve already had a thyroidectomy, in addition to making sure your thyroid medications are optimized (you will need them for life, there’s no shame in that, and you want to make sure that you are getting the optimal thyroid medications for you!), I also encourage you to take on lifestyle changes and functional medicine, to ensure that the underlying triggers that led to the development of your condition don’t lead to another autoimmune condition.
We need to rebalance the immune system to prevent this. Sometimes the autoimmunity can be reversed as well! The gut determines your immune system. With the exception of discussing proper thyroid medication dosing, the majority of my website and my book focuses on balancing the immune system. The info I present is based on my own research and journey for overcoming my autoimmune thyroid condition. Here are some articles you might find helpful:
IMPORTANCE OF GUT HEALTH
https://bruno-michael-wentz.dev01.rmkr.net/articles/importance-gut-health/
DOSE OF THYROID MEDICATION CAN UNCOVER YOUR ROOT CAUSE
https://bruno-michael-wentz.dev01.rmkr.net/articles/the-dose-of-your-thyroid-medication-can-uncover-your-root-cause/
WHERE DO I START WITH HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/where-do-i-start-with-hashimotos/
Hi! Dr. I Will like to know, how can you treat TPO antibodies so you can “stay” pregnant? How TPO antibodies affect pregnancy? Thank you!
Catalina – thank you so much for reaching out and sharing! These are some great questions! I have a list about how to optimize fertility in my Pregnancy article, such as ensuring your TSH is under 2 μIU/mL, cutting reactive foods, such as gluten, dairy and soy, optimizing your hormones, and supporting your adrenals. You will find so much more information in this article.
PREGNANCY
https://bruno-michael-wentz.dev01.rmkr.net/articles/pregnancy-announcement/
Hello Dr. Wentz,
I trust that you are well! Thank you so very much for all of the information you provide in your blogs. Your information is outlined beautifully and you most certainly have a special gift for writing! I purchased The Thyroid Secret recently and plan to get busy listening/reading. I have recently been diagnosed with hypothyroidism but no autoimmune disease after feeling like I’ve had issues for years. I am attempting to understand my lab results based on your kind information above but I’m not sure how to interpret. Thyroid brain….My TSH is 4.09, T3 is 2.9 pg/ml and T4 is 1.06 ng/dl. If I’ve done the calculations correctly to pmol/l, my T3 and T4 are way off as well as my TSH. It appears that my T3 is elevated and T4 is low? I am working with a functional medicine provider but it helps for me to have an understanding before I sit down with her. Are you able to comment?
Tracie – you are very welcome! ❤️ I’m so glad you have found a practitioner to work with you. Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication.
Izabella – thank you for all you do! I am on T3 monotherapy due to T4-T3 conversion issues, and will be testing my thyroid antibodies soon as it has been a few years. Would you recommend testing my T4 and T3 in this case, or will those results be skewed or not helpful? Thanks in advance.
Marsha – thank you for reaching out. These are the recommended thyroid function tests: TSH, TPO Antibodies, Thyroglobulin Antibodies, Free T4, Free T3, Reverse T3 (optional) and Thyroid Ultrasound (optional) If you take a T3 medication, T3 has a shorter half-life so your blood work may not be reflected accurately. It will appear that you have more thyroid hormone on board than you do. Thus it may be helpful to delay your morning dose of a T3 medication until after you do the test to see (try to schedule the test in the morning). I hope this helps and please keep me posted on your progress. ❤️
Hello,
I am concerned about taking medication to treat my elevated FSH as I have read that it can cause a dependency upon the meds and this leads to inability of the body to regulate the thyroid itself. Naturally, this sounds very scary and off-putting! I wanted to know: 1. Does taking the meds = dependency upon them? 2. If not, and you have come off the meds, when did you decide it was the right time?
MrsK – If you have subclinical hypothyroidism, it’s a gray area for treatment. For me, this is the way I think about it: if you don’t have any symptoms and you are trying to reverse Hashimoto’s the natural way, you can give yourself three months or so to get into remission. But, if you continue to worsen, and if it doesn’t get better, then I would start considering medications. Medications can help reduce many patients’ symptoms. They may also help reduce thyroid antibodies. In people who have really high antibodies or who have a lot of symptoms and antibodies, it may be a good idea to get on medications right away. There are quite a few options for thyroid medications. In my experience, what works for one person may not work for another. If your doctor will not prescribe the medication you are looking for, you may consider asking your local pharmacist for doctors in your area who prescribe the medication you are looking to try. I’m a big fan of using everything we can to get ourselves better, and medications are not always life-long. Some people are able to get off of them if they figure out their triggers and root causes. Here is an article you might find helpful:
MEDICATIONS FOR HASHIMOTO’S AND HYPOTHYROIDISM
https://bruno-michael-wentz.dev01.rmkr.net/articles/medications-for-hashimotos-and-hypothyroidism/
Thank you so much for this info and I’ve recently purchased and read your book and I’m in the midst of the beginning the protocol. That said, I’m really trying to get to your optimal reference ranges but wanted to see what your thoughts are on these results since some of the measurements appear different? For example pmol/L vs pg/mL or ng/mL.
I’ll be sure to dive in deeper with my doctor as well, just would love some guidance into what to look into further or discus.
TSH – 3.15 uiU/mL (hoping to up dosage to get to below 1.0 as you mentioned
Triiodothyronine (T3), Free — 3.7 pg/mL
Thyroxine (T4) Free, Direct— 1.55 ng/dL
Thyroixine (T4) — 6.8 ug/dL
Reverse T3, Serum — 23.4 ng/dL
Thyroxine Binding Globulin — 12 ug/mL
Thyroglobulin Antibody — 3.1 IU/mL
Thyroid Peroxidase Antibodies (TPO) — 297 IU/mL
Thank you so much!
Matt- thank you for reaching out. ❤️ Hashimoto’s is often a combination of food sensitivities, nutrient deficiencies, adrenal issues, gut issues as well as an impaired ability to get rid of toxins. Any of those things would prevent a person from getting better. Hashimoto’s is very much an individual condition. While there are root cause commonalities, each person will have their own or in some cases, more than one root cause. You will have to start with the simplest modifications, by removing triggers, followed by repairing the other broken systems to restore equilibrium, allowing the body to rebuild itself. You will need to dig down to why the immune system is imbalanced in the first place and this will tell you how you begin to finally feel better, reduce your thyroid antibodies and even take your condition into remission. You will have to create your own health timeline. Look back at your overall history as far back as you can remember. Look for infections, periods of severe stress, the use of medications (especially antibiotics, antacids, and oral contraceptives), accidents, and exposure to toxins. These are events that may have contributed to Hashimoto’s. Once you do, you will know what types of changes you need to implement to make yourself feel better. If you need further support, please check out the list of lab tests inside the “Testing” chapter of my book, Hashimoto’s Root Cause. I also offer a 12-week program, Hashimoto’s Self Management Program. Here are some resources I hope you find helpful as well. ❤️
BUILDING YOUR OWN HEALTH TIMELINE
https://bruno-michael-wentz.dev01.rmkr.net/sample-health-timeline/
Hashimoto’s Self-Management Program
https://bruno-michael-wentz.dev01.rmkr.net/enroll-in-hashimotos-self-management/
ROOT CAUSE RESET
https://bruno-michael-wentz.dev01.rmkr.net/enroll-in-root-cause-reset/
When listing optimal T3 and T4 is that same as FT3 &FT4, in the higher end of ref range? Dr did FT4 and (not F)T3, so am looking at diff charts but most seem to be for FT’s …
Thanks
Lynn – thank you for reaching out. Different labs will have different ranges, a good general guideline is to get your Free T4 (FT4) in the top half of the range, your Free T3 (FT3) in the top half to top quarter of the range and your TSH around 1.5 or below. Hope this helps!
Based on my Ulta test results and converting the numbers to your recommendations, which I hope is correct, because my test results show ng/dL and pg/mL but your recommendations are in a different format (pmol/L)….. however it shows that I might have the central hypothyroidism. A mostly normal TSH level, although sometimes it might be a bit higher and lower at various times, but mostly normal, but a low T3 and T4.
Then I noticed: “When these levels are low, but your TSH tests in the normal range, this may lead your physician to suspect a rare type of hypothyroidism known as central hypothyroidism. I’m working on an article on this topic, so stay tuned!”
Is it too soon for me to ask how that is going? I would Google everything about it, but it looks like most of the information out there is based on traditional western medicine and not functional medicine.
I have two of your books, so perhaps I could check to see if there’s anything in there, too.
Thanks for what you do.
David – thank you for reaching out! ❤️ The research and writing process is still in progress, so I don’t have a confirmed publication date yet, but be sure you are signed up for the email list for updates on it’s release! Here is a link to sign up to my newsletter https://bruno-michael-wentz.dev01.rmkr.net/gift/
Hello,
I love your work and I am so glad that I have found you. I am checking out my labs and mine are not in the same units as you are using… So I am not sure if they are within the optimal range…
This is what mine say…
Free T3 – 2.4pg/ml
Free T$ – .83pg/dl
How do I interpret these?
My TSH is 2.1ulU/mL (so optimal in some instances)
TPO is 47.6IU/mL (not zero, but still considered remission) But I am not feeling great, I have super dry skin, puffy face, weight gain, muscle aches, etc. I take Tirosint 75.
BTW, I am in So Cal and my functional Endocrinologist retired, so I am looking for a new one, any recommendations would be great.
Warmly, Julie
Julie – thank you so much! ❤️ Different labs will have different ranges, a good general guideline is to get your Free T4 in the top half of the range, your Free T3 in the top half to top quarter of the range and your TSH around 1.5 or below. When it comes to practitioners, I believe that everyone needs to find a one that will let them be a part of the healthcare team. You want someone that can guide you, that will also listen to you and your concerns. You want someone that’s open to thinking outside of the box and who understands that you may not fit in with the standard of care. It’s a good idea to ask some standard questions when contacting a new doctor for the first time. Something else to consider is you can work with a functional doctor remotely, via Skype. You could also contact your local pharmacist or compounding pharmacy, who may be able to point you to a local doctor who has a natural functional approach. But I encourage you to keep looking for the right one for you! Here are some resources you might find helpful.
CLINICIAN DATABASE
https://bruno-michael-wentz.dev01.rmkr.net/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
COMPOUNDING PHARMACIES
https://bruno-michael-wentz.dev01.rmkr.net/database-recommended-compounding-pharmacies/
Hi Dr. Izabella,
I am working with a functional medicine doctor but I also need to be able to track my own results. The optimal lab ranges you are using are different from everywhere else. Here is what several labs are using for the following thyroid labs. I’ve used both Labcorp/Quest as well as hospital labs. :
TSH-uIU/mL vs IU/L
Free T4-nG/dL vs pmol/L
Free T3-pg/mL vs pmol/L
Is there anyway that you can post a chart that has the optimal ranges in these other units of measurements? No one seems to be using the one your are using other than for the TPO and TG antibodies.
If you can post a conversion chart, I would be so grateful or at least tell us where to find a good conversion calculator. I made a huge mistake in the beginning by not looking at the unit of measurement you were using and it did cause some problems. It is very easy to overlook that because you automatically assume that it is the same unit of measurement.
Many thanks in advance.
Mary – thank you so much for your feedback and suggestion! I will discuss this with my team and see what we can come up with! In the mean time, a good general guideline is to get your Free T4 in the top half of the range, your Free T3 in the top half to top quarter of the range and your TSH around 1.5 or below. ❤️
hi, i have gotten no help in understanding if my thyroid is under or overactive from my doctor, endo, or ENT. they all just stated its in “normal range” but im wanting to understand why my body is feeling how it is. can you explain if my TSH is .728, free T4 is .60 and T3 is 105, if that is under or overactive? thank you
Patricia – thank you for reaching out. ❤️ I understand how hard it is to find a the right practitioner. Unfortunately, I am not able to give direct medical advice or a diagnosis without a comprehensive health assessment. Most people feel best with a TSH of around 1 or lower and with a Free T4 and Free T3 in the upper half of the range. It is expected that your TSH will be very suppressed when optimal on NDT medication. How much thyroid replacement therapy is needed is unique and different for each person, so it’s important to work with a functional medicine practitioner or a doctor, who can closely monitor your dosage and your progress. Here are some resources I hope you find helpful also:
TOP 10 THYROID TESTS AND HOW TO INTERPRET THEM
https://bruno-michael-wentz.dev01.rmkr.net/articles/top-10-thyroid-tests/
WHAT TO DO IF YOUR TSH IS NORMAL AND YOU ARE ANYTHING BUT
https://bruno-michael-wentz.dev01.rmkr.net/articles/what-to-do-if-your-tsh-is-normal-and-you-are-anything-but/
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://bruno-michael-wentz.dev01.rmkr.net/articles/functional-medicine-approach-to-the-thyroid
CLINICIAN DATABASE
https://bruno-michael-wentz.dev01.rmkr.net/database-recommended-clinicians/
FIND A FUNCTIONAL MEDICINE CLINICIAN
https://ifm.org/find-a-practitioner/
What an amazing article! So much valuable information given without nickel and dimming us. Thank you for all the links to more great articles and resources. Allowing us to improve our care for patients and ourselves.
Tracy – Thank you so much!🙏🏻❤️
Hi Dr. Wentz! I am so grateful for all of your thoughtful information. You are making a huge impact on my life! Any thoughts on Total T3? I’ve asked my endo to test Free T3, but she said total was more relevant and ordered that instead. My Total T3 is 91mg/dl, up from 80 since adding Cytomel to my Levothyroxine. Any info on how I can interpret my Total T3 value on its own or in relation to my other test results? Thank you for all of your dedication!!!
Kelly – thank you so much for following. I’m so glad you are finding my research helpful. Doctors usually measure total T3 and T4, which can be misleading because T3/T4 hormones are often bound to different types of proteins and aren’t available for proper use in our body. This is why I recommend the testing in this article.
I had a total thyroidectomy in 1997 and was taking synthroid. For the past few months I did not take Amy meds until recently I feel all the symptoms plus joint pains. I went to see a doctor to have my panels checked. They came out normal, which is very shocking to me! I am currently unable to do all the things I need to get done, could not function as I should, extremely fatigued and the cold hands and feet!
A – thank you for reaching out and sharing. I’m so sorry to hear you are struggling to function. Removing the thyroid with a thyroidectomy eliminates thyroid antibodies, as there is nothing left to attack. However, life is not always roses with a thyroidectomy, as it does not remove the autoimmunity. Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Even when the thyroid is taken out surgically or treated with radioactive iodine the autoimmunity still persists in most cases. Many people will have their thyroids removed, and will develop new autoimmune disorders such as Lupus, Rheumatoid arthritis, etc. The immune system just finds a different target.
We need to rebalance the immune system. Sometimes the autoimmunity can be reversed as well! The gut determines your immune system. With the exception of discussing proper thyroid medication dosing, the majority of my website and my book focuses on balancing the immune system. The info I present is based on my own research and journey for overcoming my autoimmune thyroid condition. Here is an article you might find interesting:
IMPORTANCE OF GUT HEALTH
https://bruno-michael-wentz.dev01.rmkr.net/articles/importance-gut-health/
I got my results back and am having trouble with the conversions that you list on this article. Are you able to comment on those? I did my tests with Ulta Labs.
Free T3 2.6 pg/ml
Free T4 1 ng/dl
Thyroglobulin <1 IU/ml
TPA 1 IU/ml
TSH 1.82 mIU/ml
Are these in a normal range? When I calculated some, they seemed low (like the FT4, or am I wrong?) Thanks for any insight if you are able!
Julie – thank you for reaching out. Different labs will have different ranges, a good general guideline is to get your Free T4 in the top half of the range, your Free T3 in the top half to top quarter of the range and your TSH around 1.5 or below.
Thanks so much for this! I will take another look at them.
I love, love, love reading your articles. They are so easy to understand and so incredibly helpful.
Julie – My pleasure! It’s an honor to be a part of your journey.
Hi there,
I’m looking for a reason to test TG as well as TPO. Not seeing it. I just tested my TPO but have never tested TG and wondering if I need to.
Thanks,
Stephanie
Stephanie – Thank you for following. About 95% of people with Hashimoto’s have elevated Thyroid Peroxidase Antibodies, while 80% will have elevated Thyroglobulin Antibodies. They can both be important in monitoring the autoimmune attack on the thyroid, and can both be used to monitor the effect of interventions. Here are some articles I think you might find helpful:
HASHIMOTO’S AND THYROID ANTIBODIES: PART 1
https://bruno-michael-wentz.dev01.rmkr.net/articles/hashimotos-and-thyroid-antibodies/
HASHIMOTO’S AND THYROID ANTIBODIES: PART 2
https://bruno-michael-wentz.dev01.rmkr.net/articles/part-2-mechanisms-reduce-thyroid-antibodies/
Oh shoot! I forgot to ask you another question. How do I convert pmol to pg/ml and ng/ml?? Because that’s what my numbers are in, not in pmol.
Thanks again!
Stephanie – Different labs will have different ranges, a good general guideline is to get your Free T4 in the top half of the range, your Free T3 in the top half to top quarter of the range and your TSH around 1.5 or below.
Thank you so much for all your help in this journey! I am taking the online Root Cause class as well, and I’m finding it to be really helpful. One technical question: As I look at my results for Free T4 and T3, they are described in the units ng/DL and pg/mL, respectively. I can’t figure out how to convert them to the pmol/L units you mentioned above. Any help appreciated!
Michelle – thank you so much for sharing. It’s an honor to be a part of your journey ❤️❤️❤️ Different labs will have different ranges, a good general guideline is to get your Free T4 in the top half of the range, your Free T3 in the top half to top quarter of the range and your TSH around 1.5 or below. Please feel free to email my team at info@thyroidpharmacist.com if you have any questions.
I am wondering what can be said about elevated TSH and Free T4? Does it mean lab did a faulty test as I do not see this type in your explanations nor anywhere else except saying they took too much medications. In our case no medictions are used.
Daiva – thank you for following. It’s hard to say, I recommend discussing your concerns with your practitioner.
Hi what about Mercury Toxins in the body? That causes thyroid as well
Also how can I consult with you? I’ll be doing some of the labs indicated above can you help In interpretation???
One question does pure whey protein affect the gland?
Ana – thank you for reaching out. Toxins and chemicals are established environmental triggers for developing Hashimoto’s in people who are genetically predisposed. These include iodine intake, bacterial and viral infections, hormonal imbalances, toxins, as well as therapy with certain types of medications and mercury! When it comes to whey protein, everyone with Hashimoto’s will have some degree of intestinal permeability, which makes one’s immune system more likely to recognize whey and casein proteins as foreign invaders, and create IgG antibodies to protect itself. Here are a couple articles I hope you find helpful:
MERCURY EXPOSURE AND HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/mercury-exposure-hashimotos/
GOING DAIRY FREE TO REVERSE HASHIMOTO’S
https://bruno-michael-wentz.dev01.rmkr.net/articles/going-dairy-free-to-reverse-hashimotos/
Unfortunately, at present time I am not accepting new clients. I do offer a 12 week online program called Hashimoto’s Self-Management Program, that covers all of the strategies that I go through with my one-on-one clients, in a self-paced format, so that participants have access to all of the things I’ve learned about Hashimoto’s without having to schedule costly consults with me or another practitioner. Here is the link to the program if you are interested in checking it out:
Hashimoto’s Self-Management Program
https://bruno-michael-wentz.dev01.rmkr.net/enroll-in-hashimotos-program/
Please feel free to email my team at info@thyroidpharmacist.com if you have any questions regarding the protocols as well!
If you would like to be notified of any future consulting opportunities and educational events, you can sign up for my waiting list: https://bruno-michael-wentz.dev01.rmkr.net/dr-izabella-wentzs-waiting-list/