Thyroid cancer rates have doubled over the past thirty years and continue to climb. In fact, thyroid cancer is currently the third fastest rising cancer diagnosis in the US.
Studies have shown that Hashimoto’s patients are three times more likely to develop thyroid cancer, so it’s important to increase your thyroid cancer awareness, as most thyroid cancers can be treated successfully if diagnosed early.
Unfortunately, thyroid cancer takes 1,900 people from us on an annual basis.
At the same time, around 10,000 Americans needlessly get their thyroid glands removed due to thyroid growths that have long been misclassified as cancers, but are not actually cancerous.
While visiting Chicago last year, I spoke with Wendy, a courageous woman who had her thyroid gland removed because of suspected thyroid cancer.
Wendy was first diagnosed with hypothyroidism and Hashimoto’s and followed the “standard of care”, taking synthetic T4 medications until her doctor told her that she had thyroid cancer. Scared and confused, she followed her doctor’s advice to have her thyroid removed…
She continued to struggle for 10 years with numerous symptoms until she was frustrated to the point to take charge of her own health and sought out a doctor trained in functional medicine…
Wendy requested her previous medical records as she prepared to transition to a new doctor. It wasn’t until Wendy began reading through her medical history when she learned that, in fact, she never had thyroid cancer… she only had a thyroid nodule that was considered to be benign (not cancerous).
I want to make sure that you are properly informed about thyroid cancer, so you can make the best decision for yourself.
In the following article, you’ll discover:
- The different types of thyroid cancers: which ones are aggressive and which ones are slow-growing?
- The important reclassification of certain thyroid growths that were once considered thyroid cancer and should not require removal of your thyroid gland!
- Factors that can increase your risk of thyroid cancer
- What the research is saying about thyroid cancer prevention…
- What to do if you’ve already had your thyroid gland removed because of suspected thyroid cancer (or something else)
History of Thyroid Cancer
Thyroid cancer rates have doubled over the past thirty years and continue to climb, making it the most rapidly increasing cancer in the US. Estimates for 2017 by the American Cancer Society show that thyroid cancer diagnoses continue to rise. Even with this increase, death from thyroid cancer is low compared to most other cancers.
Dr. Steven Eisenberg, an oncologist who specializes in thyroid cancer, reported that there are approximately 62,450 cases of thyroid cancer per year and that 45,000 of those are women. Sadly, 1,900 per year lose their lives to thyroid cancer on an annual basis.
Overdiagnosis Controversy
Some experts in the field believe the increase is due to the widespread use of ultrasounds and other imaging studies that find nodules that would not otherwise be found, and that this technology detects growths that are incorrectly classified as cancers, or cancers that have a very low chance of actually progressing or causing harm during the person’s lifetime.
A recent initiative by the National Cancer Institute sought to reclassify one type of papillary thyroid tumor from being considered cancerous (encapsulated follicular variant of papillary thyroid carcinoma) to a non-invasive tumor (non-invasive follicular thyroid neoplasm with papillary-like nuclear features). This type of tumor is encapsulated by scar tissue and is not likely to spread or progress.
They felt giving a ‘cancer’ diagnosis should be reserved for conditions that have a realistic probability of fatal progression. However, this type of papillary cancer did not have a high likelihood of progressing to thyroid cancer, and instead often resulted in psychological distress for patients, as well as unnecessary removal of the thyroid gland or radioactive iodine in many cases.
The reduced psychological effect to patients is enormous. Just saying the “C-word” has a big impact on a patient’s decisions about their health, often resulting in the ‘fear factor’ driving those decisions. This reclassification is estimated to affect about 10,000 of the 65,000 thyroid cancer cases diagnosed each year, meaning that currently has many as 10,000 people each year may be having their thyroid glands removed or treated with radioactive iodine!
Therefore, if you’re ever told that you have “thyroid cancer”, you need to ask questions about the specific type of cancer it is, and in some cases even get a second opinion to ensure that you are getting the right diagnosis and the right treatment.
There are numerous kinds of thyroid tumors—some can be aggressive and require aggressive treatment. Others can be benign.
Thyroid Growths
Tumors are often identified after looking for nodule growths that may appear on the thyroid, so it’s important to understand thyroid nodules.
When using advanced diagnostic methods such as high-resolution ultrasonography, 20 to 76 percent of the general adult population may have thyroid nodules, and thyroid nodules are also more common in people with Hashimoto’s.
For the most part, the nodules are very slow growing and can take decades before symptoms appear or are noticed. Most of these nodular growths do not cause any symptoms at all and would go unnoticed without technology. People who have elevated antibodies or a thyroid that appears larger than normal during a routine physical exam by a practitioner may be recommended to have an ultrasound of their thyroid.
Most nodules are benign (read: non-cancerous); however, thyroid cancers generally begin with a nodule and 1 to 2 percent of nodules may be cancerous, so if you have a thyroid nodule, it’s important to get an accurate diagnosis.
Additionally, some nodules make extra thyroid hormone and can cause hyperthyroidism. These nodules are generally non-cancerous, but in Wendy’s case, her thyroid hormone producing nodule was misdiagnosed as cancer and led her to have her thyroid gland removed.
Screening for Thyroid Cancer
When a practitioner suspects a patient may have nodules on the thyroid, an ultrasound of the thyroid is usually ordered. Through this process, the radiologist who reads the ultrasound will identify and clearly mark any nodules found.
There are certain characteristics that an oncologist (a doctor specializing in cancer) will look for in regards to the size, shape, and location of nodules. If any nodules are found to be concerning, a biopsy with fine needle aspiration (FNA) may be requested. A tiny needle is used to remove some of the cells from a suspected nodule to be looked at with a microscope. While FNA can identify papillary thyroid cancers, this process is not helpful with follicular thyroid cancer which requires a post-surgical evaluation of the thyroid tissue to determine if cancer is present.
Other diagnostic approaches that are under investigation include the use of positron emission tomography (PET) scans and cellular and molecular markers. Recently, a group of Canadian scientists discovered a protein marker that could help identify whether a papillary nodule is aggressive or benign. If a nodule is labeled as benign, there is currently no harm associated with the growth or tissues.
Other tests include thyroid scintigraphy (a scan with radioactive iodine) to assess thyroid nodules, which has become less common over the past ten years. Although scintigraphy remains the only way to determine the functional status of a nodule, high-resolution ultrasound of the thyroid is superior in identifying the physical characteristics of the thyroid. Patients who have a low serum thyroid stimulating hormone (TSH) concentration may benefit more from having the scintigraphy to exclude an individual functioning hot nodule, which would be less likely to be malignant.
Is Thyroid Cancer Really the Best Cancer to Have?
I’ve often heard from patients who confide that their doctors told them their diagnosis of thyroid cancer was the best type of cancer to have! I don’t think any cancer is a good cancer to have, though it is true that many types of thyroid cancer are slow growing and 5 year survival rates of people diagnosed with thyroid cancer are 98 percent. There is also data that suggests many types of thyroid cancers are so slow growing and not likely to cause problems that up to a third of older adults who died of other causes are found to have a low grade thyroid cancer on autopsy! An increase in screening is finding these low grade cancers earlier in life and patients are told to treat the cancers when in many cases, the person could live a full life without the cancer ever spreading or creating any health challenges for them.
However, I think that it’s also important to note that while rare, some thyroid cancer variants may be aggressive.
Aggressive Cancer Characteristics
More aggressive cancers are likely to be noted by rapidly enlarging neck mass, neck pain and tenderness, shortness of breath or difficulty breathing, difficulty swallowing, hoarseness, and a cough (and sometimes coughing up blood).
While less common, other symptoms can include chest pain, bone pain, headache, confusion, or abdominal pain from cancer spreading to that part of the body.
Other symptoms may be weight loss, fatigue, or a fever of unknown origin. Again, proper diagnosis is important. Discuss any symptoms you may be experiencing with your health practitioner.
Types of Thyroid Tumors
There are three main types of thyroid tumors:
- Differentiated (includes papillary, follicular and Hürthle cell)
- Medullary
- Anaplastic
Differentiated
Differentiated tumors look a lot like normal thyroid tissue under a microscope and arise from thyroid follicular cells, which are located on the surface membrane lining of the thyroid gland. There are several types of differentiated thyroid cancers. Most are slow-growing and can be treated effectively with early diagnosis.
The different types of differentiated tumors are:
- Papillary – This is the most common type of thyroid cancer, making up as much as 90 percent of all thyroid cancer diagnoses. These tumors arise from the membrane lining of thyroid tissues and appear as finger-like projections of abnormal growths with a fibrous core. Papillary cancers are rarely fatal and can be effectively treated with proper diagnosis. They are slow-growing and are usually present in only one lobe of the thyroid gland. Additionally, some of these tumors may not actually be cancerous, based on the recent reclassification mentioned above, so it’s always important to ask questions.
- Mixed papillary-follicular variant – Subtypes of papillary cancers have similar positive outcomes when found early.
- Various subtypes – columnar, tall cell, insular, and diffuse sclerosing – These subtypes are not as common and tend to grow and spread rapidly, so more aggressive treatment options may be indicated.
- Follicular cancers – These types of cancers make up about 10 to 14 percent of all thyroid cancers. They may be referred to as follicular carcinoma or follicular adenocarcinoma. Countries, where diets are lacking in iodine, have higher rates of this particular thyroid cancer. While this type of cancer is more aggressive compared to papillary cancers, most cases still have positive results. This type of cancer does not spread to the lymph nodes but can spread to other areas of the body such as the lungs or bones.
- Hürthle (Hurthle) cell cancer – This is a rare cancer that is often difficult to discover and treat. About 3 percent of thyroid cancers make up this type. It is also known as oxyphil cell carcinoma.
Medullary thyroid cancer (MTC)
Medullary thyroid cancer is a rare but aggressive cancer that makes up about 4 percent of all thyroid cancers. This type develops from the C cells in the thyroid gland, which produce calcitonin, which controls calcium levels in the blood. This type will sometimes spread to lymph nodes, lungs, or even the liver before a nodule is diagnosed.
There are two types of medullary thyroid cancers:
- Sporadic MTC – This type of cancer occurs mostly in older adult populations and is found in only one lobe of the thyroid. It is not an inherited disease and accounts for about 80 percent of all cases of MTC.
- Familial MTC – This type of thyroid cancer is passed on between family members and often develops in childhood or in the early adult years. Both lobes of the thyroid gland are usually affected. This type is often connected with an increased risk of other types of cancers.
Anaplastic (also called undifferentiated carcinoma)
Anaplastic cancer is rare (less than 2 percent) and can be very aggressive. This type of thyroid cancer is thought to develop from existing papillary or follicular cancers.
Less common thyroid cancers – Thyroid lymphomas and thyroid sarcomas are rare but should be included as part of a complete diagnosis.
Parathyroid cancer – The parathyroids are not part of the thyroid gland at all, but are attached to the gland itself. Since nodules can develop on these tiny glands near the thyroid gland, they are included here. This type of cancer is very rare (less than 100 cases in the US each year). The standard of care treatment for this type is surgical removal.
What is the Current Standard of Care?
People who are found to have benign nodules are monitored on an annual basis with an ultrasound and generally surgery is not recommended, unless the nodules are painful or causing symptoms. (Side note: I have case studies and stories of people using the strategies in Hashimoto’s the Root Cause and Hashimoto’s Protocol who have had their benign nodules shrink or go away entirely!)
The current standard of care treatment options for thyroid cancer can include: surgery to remove the full or partial thyroid gland, radioactive iodine treatments, external beam radiation, chemotherapy, targeted therapy, and thyroid hormones. Often times, a couple of the options may be used together.
In addition to numerous side effects, the consequences of both radioactive iodine and removal of the thyroid gland is the lifelong requirement of external thyroid hormones. In many cases, people are not dosed on thyroid hormones correctly and go on to struggle with thyroid symptoms.
Furthermore, removing the thyroid gland may still leave an immunological imbalance in the body that led to the development of autoimmune disease or cancer in the first place.
Thyroid Cancer Causes and Risks
Environmental issues
Scientists have found that incidence rates of thyroid cancer are reported to vary in different regions of the world. For example, in 2013, Iceland and Hawaii were reported to have double the rates of thyroid cancer compared to Northern European countries, Canada, and the rest of the USA.
In Hawaii, the rates of cancer are higher in each ethnic group compared to the incidence rates of those ethnic groups in their countries. According to www.thyroidmanager.org, Chinese males and Filipina females in Hawaii have the highest rates of cancer. In 2014 and 2016, researchers reported that California had higher rates of aggressive and advanced thyroid cancers compared to the rest of the United States.
Interestingly, areas with volcanic activity, the Philippines, Hawaii and Iceland, have the highest rates of thyroid cancer. Vanadium, a metal component of volcanic ash, is suspected.
The risk factors that have been identified for cancer in general include: aging, genetics, radiation, toxins, certain viruses and bacteria, hormones, diet, obesity, air and water pollution, smoking, and alcohol intake (causes 3.6 percent of all cancers).
For thyroid cancer specifically, Hashimoto’s has also been implicated as a risk factor.
Since we don’t have a way to stop aging yet, let’s focus on how we can modify our other risks… (I’m going to skip the discussion on smoking, as this to me is an obvious no-no for any person who wants to be healthy!)
Genetics
While there are many genes implicated in cancers, and I don’t typically focus on genetics too much, I do want to highlight the role of the common MTHFR gene variation. This is because we know how to modify this gene, so that we don’t suffer consequences from having it! This gene variation is present in about 50 percent of the population, thus many people with Hashimoto’s have the MTHFR (Methylenetetrahydrofolate Reductase) gene variation. A recent study identified that one type of variation of this gene (MTHFR C677T) is linked to developing thyroid cancer. A blood test is available to give you the information you need to know about your risk and how you can best support your health. Having this altered gene can also make it difficult for one to process folic acid. Some professionals claim that the type of folic acid added to cheap supplements and processed foods may even create a toxic buildup in the body. This may explain why studies have shown that folic acid supplements may increase cancer risk!
One US based study found that subjects taking a multivitamin at least weekly for more than 10 years showed an increased rate of both thyroid and papillary cancer!
Generally, most multivitamins available in 2002 contained folic acid, and most of the typical drugstore brands still do! Thus, I recommend ditching cheap multivitamins! Instead, a methylated folate supplement may be helpful for people with the MTHFR gene variation. MTHFR Pathways contains methylated folate.
While some thyroid researchers keep finding more and more genes that lead to autoimmune and thyroid cancer development, I think that we need to pay less attention to genes, and more attention to the environment. After all, we can’t change our genes, but we can change our environment, and new research in the field of epigenetics is now showing that environmental factors can determine the expression of genes.
Perhaps the best way to demonstrate the impact of environment on thyroid cancer is through the effect of toxic radiation, as seen in the Chernobyl tragedy.
Radiation Exposure
I don’t have a personal history of thyroid cancer, but having been exposed to the Chernobyl nuclear disaster at age three, this subject is close to my heart. People who lived in close proximity to the nuclear disaster ended up with higher rates of Hashimoto’s, benign thyroid growths, as well as cancerous thyroid tumors (specifically papillary cancers). Thyroid cancer among exposed children was the most significant health impact of the disaster; an excess of 6,000 cases of thyroid cancer was reported up to 2005, from the fallout!
A 2003 review of the implications of radiation on autoimmune thyroid disease in the journal Thyroid found that even though they were otherwise genetically and culturally similar, 81 percent of children who lived in a contaminated region of the Ukraine after the Chernobyl nuclear disaster had thyroglobulin antibodies, compared to only 17 percent of children living in another part of Ukraine that were further away from the nuclear disaster.
While previous studies implicated just high doses of radiation as problematic, new studies show that even low doses of radiation have been found to modulate the immune system. This immune modulation can diminish some autoimmune conditions (rheumatoid arthritis, lupus, multiple sclerosis, atopic dermatitis), but at the same time exacerbate others (asthma and Hashimoto’s). The data is controversial whether low doses of radiation can contribute to thyroid cancer, but I still recommend that you are properly protected when you have to have medical or dental x-rays. You can request coverage of your neck using a thyroid shield whenever you get any x-rays (both medical and dental). Limiting radiation can potentially protect you from both thyroid cancer and Hashimoto’s…
This brings me to the next risk factor for thyroid cancer: Hashimoto’s.
Hashimoto’s and Thyroid Cancer
Hashimoto’s patients are three times more likely to develop thyroid cancer. While many factors may lead to the development of thyroid disease, thyroid nodules, tumors and cancers, let’s look at how you can take charge of the things you can cantrol.
Hashimoto’s increases the risk for thyroid cancer, and an elevation in thyroid antibodies may indicate a potential risk for thyroid cancer as well. Elevated thyroglobulin antibodies (TGAb) have been associated with an increased risk of certain thyroid cancers.
Over the last few years, I have found that thyroglobulin antibodies, which have been implicated in Hashimoto’s, Graves’ and thyroid cancer, usually develop before TPO antibodies, cause anxiety, and are related to radiation and toxicity.
Scientists suggest that the chronic inflammation associated with Hashimoto’s is a risk factor for cancer development. Therefore, addressing your Hashimoto’s and thyroid antibodies should in theory lower your risk of certain types of thyroid cancer as well.
I’m happy to report that although my thyroglobulin antibodies were over 800 when I first learned I had Hashimoto’s, they have been consistently testing at 0, or <1, in every test over the last five years!!
The research in Hashimoto’s the Root Cause, Hashimoto’s Protocol and essentially this entire website is dedicated to giving you strategies to take back your health with Hashimoto’s!
Toxins
I’ve written extensively about toxins in our food sources, air, water systems, and personal care products and their connection to Hashimoto’s…
Environmental toxins in general have also been tied to various cancers and autoimmune disease, while Agent Orange, heavy metals, perchlorates, flame retardants, and pesticides have specifically been implicated as potential triggers for thyroid cancers…
- Chemicals used in industrial and construction materials, such as PCB’s (polychlorinated biophenyl), arsenic, benzene, chromium, ethylene oxide, nickel, polonium, vinyl chloride, formaldehyde, toluene, plastics, detergents, chloroform, petroleum, fertilizer, sulfur oxide, pesticides, and trichloroethylene are potentially carcinogenic.
- Various toxins such as ammonia, radioactive decay, methane, and hydrofluorocarbons can be found in our air supply, while oils, plastics, detergents, halogens and pesticides can pollute our water supply.
- Chemicals found in conventional personal care products including: dioxane, petrolatum, formaldehyde, synthetic fragrance, talc, parabens and phthalates are considered to be carcinogenic.
Scientists believe that people with genetic variations that prevent them from properly clearing certain toxins are thought to be at increased risk, and there is evidence that nutrient deficiencies play a role in improper detoxification. I’ve found that those with genetic variations can benefit from targeted high dose nutrient therapy.
Some strategies that may be helpful for addressing toxicity include:
- Supporting your body’s detoxification pathways with targeted nutrients, antioxidants, herbs and supplements. Selenium, Vitamin C, Polyphenols and flavonoids are some examples. For people with thyroid disease, I recommend a small dose of selenium 200 mcg on a daily basis, and I recommend a 1-2 week liver support cleanse (such as the Rootcology Liver Support Kit) at least once or twice each year.
The Rootcology Liver Support Kit includes:
- MTHFR Pathways – This maintains a healthy homocysteine pathway. An optimally functioning homocysteine pathway provides methyl and sulfur groups for biochemical reactions such as detoxification, healthy immune function, brain, and cardiovascular health.
- Liver Reset – This contains a natural pea protein isolate to fuel natural detoxification pathways. It includes the nutrients needed to support and balance phase I and II metabolic pathways, high levels of antioxidants for safe detoxification, and a comprehensive array of herbal hepatics and cholagogues to promote healthy liver function and elimination.
- Liver & Gallbladder Support – This is a comprehensive formula designed to support bile flow for the normal processing and elimination of toxins through the specific combination of nutrients and herbs in this formula. By supporting liver and gallbladder function, Liver & Gallbladder Support™ supports the elimination of fatty substances from the liver and the digestion and assimilation of fats and fat-soluble vitamins.
- Amino Support – This is useful for preparing the liver for phase II detoxification. Providing nutritional support for phase II detoxification helps conjugate toxins and prepare them for safe elimination from the body.
- NAC – NAC supports tissue levels of glutathione, a key component of the antioxidant defense system.
- Magnesium – Magnesium activates the enzymes necessary for a number of physiological functions, including neuromuscular contractions, cardiac function, and the regulation of the acid-alkaline balance in the body. It is necessary for the metabolism of carbohydrates, amino acids, and fats; also for energy production, and the utilization of calcium, phosphorus, sodium, and potassium. This vital mineral also helps utilize B-complex vitamins, vitamin C, and vitamin E.l.
For more information regarding the Liver Support Protocol and these supplements, check out my article on how to support your liver to rid your body of toxins, here!
2. Getting a water filter that removes toxins from the water supply. I have the AquaTru filter in my bathroom, so I always have access to clean water. (The AquaTru filter is the only countertop reverse osmosis filter that removes not just toxins, but also fluoride, a chemical that can suppress thyroid function).
3. Purifying your air supply. I use the AirDoctor in my bedroom to purify the air.
4. Investing in clean versions of personal care items. Some of my favorite brands are Annmarie Skin Care, Acure and SpaDr. I’ve also written an extensive article on personal care products.
5. Sweat therapy! Sweating is a great way to get rid of toxins! I like hot yoga, hot Epsom Salt baths or using a sauna to get the sweat out. I have a Sunlighten sauna in my basement 🙂 However, please note that sauna use may not be recommended in specific circumstances, or for those with certain medical conditions. You can learn more about infrared sauna contraindications in my article on saunas and Hashimoto’s.
Nutrition
Research has also shown potential cancer-preventing benefits in the following nutritional interventions.
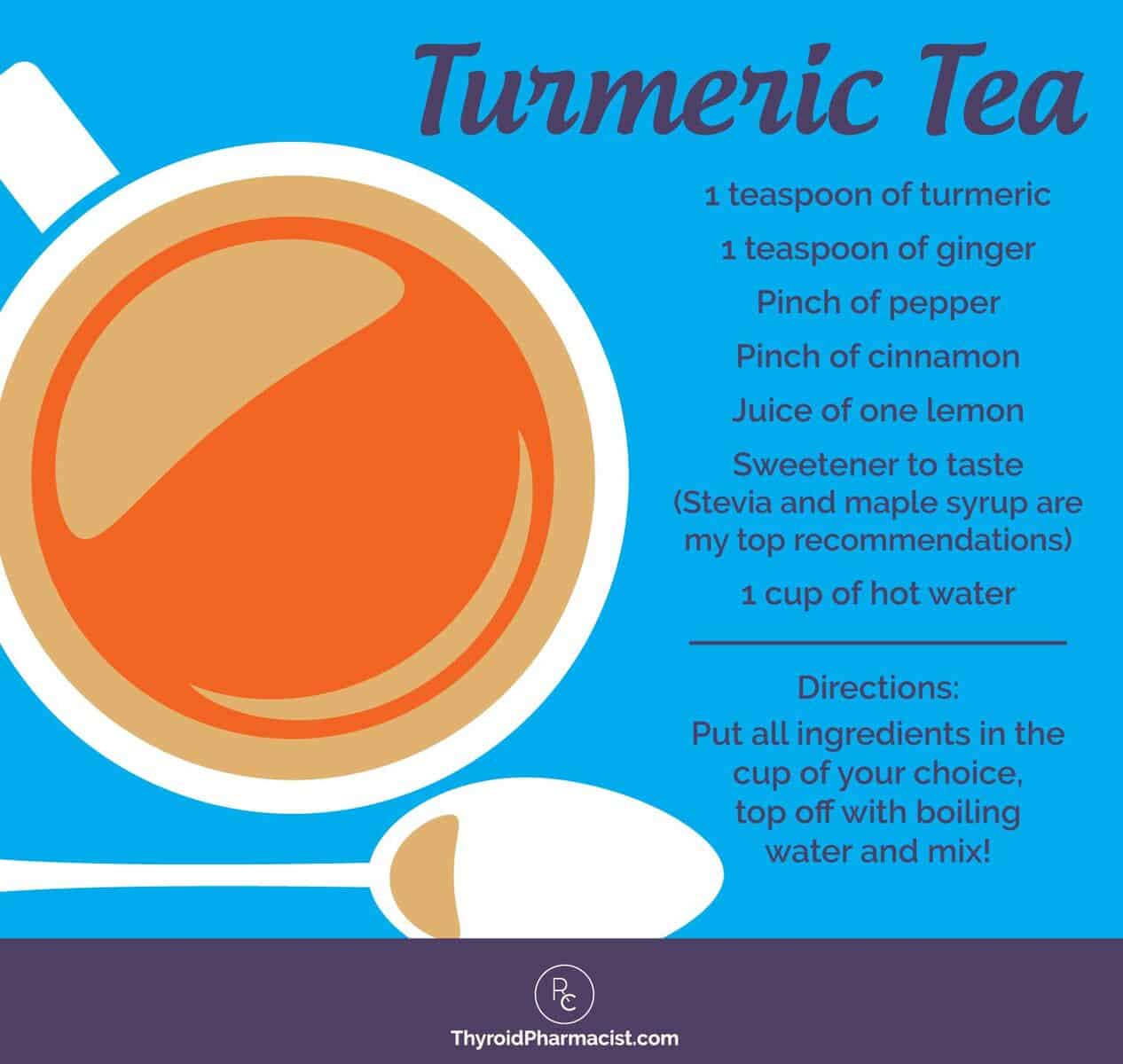
Turmeric
Turmeric is known for fighting inflammation and may even have tumor inhibiting activity in thyroid cancer! Turmeric can also be a helpful supplement to help with clearing out toxins. According to a 2014 study in the journal Food Chemistry and Toxicology, “curcumin reduces the hepatotoxicity induced by arsenic, cadmium, chromium, copper, lead and mercury, prevents histological injury, lipid peroxidation, and glutathione (GSH) depletion, maintains the liver antioxidant enzyme status and protects against mitochondrial dysfunction.”
In a previous blog post, I spoke about turmeric and how adding this spice into your diet and care could provide a host of benefits. Curcumin is the active ingredient in turmeric and is what gives turmeric its golden color. Remember that turmeric leaves the body quickly, and it’s important to combine with other foods to extend the benefit as well as taking a high-quality supplement.
My preferred curcumin supplement is this one from Rootcology.
You can also try this tasty tea recipe, to incorporate more turmeric into your diet:
Resveratrol
Resveratrol, which can be found in red wine, has received lots of recognition in recent years as a wonder ingredient. This might explain why one study found that females who consumed more than 3 glasses of wine per week had a decreased risk of papillary thyroid cancer when compared with non-drinkers. Of course, drinking wine for health prevention is a bit controversial… Other studies have found that having two or more daily drinks over the course of years increases the risk of mouth, throat, esophagus, stomach, liver, colon, lymphomas, prostate, kidney, breast and ovary cancers.
Additionally, excessive alcohol intake can lead to alcoholism, toxicity, blood sugar imbalances and dysbiosis in the susceptible individual… For some people, 3 glasses of wine per week may be too much! If you do choose to drink wine, I prefer Dry Farms wine for a less toxic version.
If you’d rather forgo the wine, you can also get Resveratrol as a supplement.
Fruit and Vegetables
Countless studies have shown that diets containing high amounts of fruits and vegetables with active micronutrients and phytochemicals provide antioxidants which protect against many types of cancer; however, there are some fruits and vegetables that have been found to play a protective role against thyroid cancers specifically. These fruits and veggies include: fresh tomato, lemon, persimmon, tangerine, cassava (I like Otto’s Cassava as a gluten-free baking flour), turnips and rutabagas. Including these specific fruits and vegetables regularly and often in your diet is recommended to boost your body’s thyroid cancer fighting abilities.
While a high consumption of fruits and vegetables has been found to be beneficial for cancer prevention, there are a few vegetables that may actually increase the risk of thyroid cancer. Cruciferous vegetables such as brussels sprouts, cabbage, and broccoli have been found to contain a form of thioglucosides, which may increase thyroid cancer risk by inhibiting iodine transport to the thyroid gland. The risks seem to be increased in countries with iodine deficiencies; none of the studies were done in the United States.
Iodine
Iodine, while a controversial nutrient in thyroid disease in general, seems to have a goldilocks relationship with thyroid cancer as well.
While studies report that overall thyroid cancer rates are not affected by dietary iodine intake, the types of cancers that occur in low iodine intake areas vary from the types of cancers that occur in areas with high intake.
In general, I recommend the amount of iodine in multivitamins, but not much higher for people with Hashimoto’s and those who are looking at preventing thyroid cancer. Read my iodine article here.
Teas
Even certain herbal teas can have a positive or negative effect on thyroid health. For example, in one study, high green tea consumption was found to increase thyroid cancer risk in premenopausal women; however, it can decrease the risk in postmenopausal women.
Consumption of chamomile tea, however, has been shown to protect against not only thyroid cancer, but also against other types of thyroid conditions as well!
Fish/Omega-3 Fatty Acids
Many studies have also found that a higher consumption of fish, in general, is a favorable indicator of the risk of several cancers. However, there are some fish that can combat certain thyroid cancers specifically. For example, one study found that in 82 percent of cases, frequent intake of saltwater fish decreased papillary thyroid cancer risk in adult females.
In addition, patients dealing with thyroid cancer will benefit from including essential fatty acids and omega-3’s into their diets.
Weight
While there are some risk factors for thyroid cancer you cannot change such as genetics, age and gender, there are some risk factors, such as being overweight or obese, that you can change. One meta-analysis found that being overweight, obese or having an unhealthy BMI were all associated with an increased risk of thyroid cancer.
Researchers found:
- Each 5-unit increase in BMI was associated with a 30 percent increased risk.
- Each 5-kg increase in weight was associated with a 5 percent increased risk.
- Each 5-cm increase in waist or hip circumference was associated with a 5 percent increased risk.
- Each 0.1-unit increase in waist-to-hip ratio was associated with a 14 percent increased risk.
Reducing stress, improving your outlook on life, increasing your physical activity, and reducing your waistline are some steps you can take to enhance your healing journey.
I’ve also written a comprehensive article on losing weight with Hashimoto’s.
What to Do if You’ve Already Had Radioactive Iodine or Your Thyroid Removed Due to Thyroid Cancer?
First and foremost, if you’ve had treatment for thyroid cancer that took out a part or all of your thyroid gland or destroyed the thyroid cells, you will need to focus on optimizing your thyroid medications. I’ve seen dangerous suggestions from people who claim to be thyroid experts that one can live without taking thyroid hormones, even after having their thyroid gland removed! Please don’t listen to these suggestions, as thyroid hormones are required for life! I’ve written extensively about thyroid medications. Generally, people who have had their thyroid gland removed will need higher doses, and may even need a mixture of thyroid hormones, such as T3/T4 thyroid meds. You can read more about thyroid meds in my article: Which Thyroid Medication Is Best?, and I also have an eBook you can download for free called Optimizing Thyroid Medications.
Second, most thyroid conditions (Hashimoto’s, Graves’, thyroid cancer) result from an immune system that is out of balance. This can be caused by nutrient deficiencies, food sensitivities, toxins, a gut imbalance, poor stress response and/or chronic infections. Even when the thyroid is taken out surgically or treated with radioactive iodine, the immune imbalance still persists in most cases, and a person may go on to develop additional health conditions, and still feel unwell. This is why it’s important to take charge of your health and lifestyle. My work on this website and in my books Hashimoto’s Root Cause and Hashimoto’s Protocol has helped many people post RAI and thyroidectomy, and I hope that it will also be helpful on your journey!
Be Your Own Best Advocate
I have had the pleasure of working with many women and men to help them find the right answers on their journey back to health. Some have experienced success with alternative therapies. Many have seen their health improve and their nodules shrink or diminish through natural methods including acupuncture, the Autoimmune Paleo diet, taking a low dose of thyroid hormones and treating any infections you may have, like H Pylori, which has been linked to nodules. (I will be writing an article on shrinking nodules soon as well.)
One of the most important things you can do is to educate yourself properly. Of course, I concur wholeheartedly. My own path to healing from Hashimoto’s resulted in my trying many different approaches, often being a guinea pig to myself as there just weren’t enough resources available at the time.
Knowledge equals power. Arming yourself with information about how your body works is one of the best defenses you can have to prevent thyroid cancer and heal. Let go of the “fear factor” and embrace that even if faced with something as damaging as thyroid cancer, it’s not always a death sentence. There are many paths to healing, and empowering yourself with knowledge is the most important step towards healing.
References
- Popoveniuc G, Jonklaas J. Thyroid Nodules. The Medical clinics of North America. 2012;96(2):329-349. doi:10.1016/j.mcna.2012.02.002.
- The American Cancer Society medical and editorial content team. What Is Thyroid Cancer? https://www.cancer.org/cancer/thyroid-cancer/about/what-is-thyroid-cancer.html. Published April 15, 2016. Accessed October 20, 2017.
- The American Cancer Society medical and editorial content team. About Thyroid Cancer PDF. https://www.cancer.org/content/dam/CRC/PDF/Public/8853.00.pdf. Published April 15, 2016. Accessed October 20, 2017.
- The American Cancer Society medical and editorial content team. Signs and Symptoms of Thyroid Cancer. https://www.cancer.org/cancer/thyroid-cancer/detection-diagnosis-staging/signs-symptoms.html. Published April 15, 2016. Accessed October 20, 2017.
- The American Cancer Society medical and editorial content team. About Thyroid Cancer PDF. https://www.cancer.org/content/dam/CRC/PDF/Public/8853.00.pdf. Published April 15, 2016. Accessed October 20, 2017.
- The American Cancer Society medical and editorial content team. Treating Thyroid Cancer PDF. https://www.cancer.org/content/dam/CRC/PDF/Public/8856.00.pdf. Published April 15, 2016. Accessed October 20, 2017.
- Welch G, Woloshin S, Schwartz L. Overdiagnosed: Making People Sick in the Pursuit of Health. 1st ed. Boston, MA: Beacon Press; 2011.
- Morris L, Sikora A, Tosteson T, Davies L. The increasing incidence of thyroid cancer: the influence of access to care. Thyroid. 2013; 23(7):885-891. doi: 10.1089/thy.2013.0045.
- Nguyen Q, Lee E, Huang M, Park Y, Khullar A, Plodkowski R. Diagnosis and Treatment of Patients with Thyroid Cancer. American Health & Drug Benefits. 2015;8(1):30-40.
- Lubitz C, Kong C, McMahon P, Daniels G, Chen Y, Economopoulos K, et al. Annual financial impact of well‐differentiated thyroid cancer care in the United States. Cancer. 2014;120(9):1345-1352.
- Chen Y, Lin C, Cheng F, Sung F, Kao C. Cancer risk in patients with Hashimoto’s thyroiditis: a nationwide cohort study. British Journal of Cancer. 2013;109(9):2496-2501. doi:10.1038/bjc.2013.597.
- Chen Y, Wang B, Yan S, Wang Y. Significant association between MTHFR C677T polymorphism and thyroid cancer risk: evidence from a meta-analysis. Genetic testing and molecular biomarkers. 2014;18(10):695-702. doi:10.1089/gtmb.2014.0029.
- Qin J, Yu Z, Guan H, Shi L, Liu Y, Zhao N, et al. High thyroglobulin antibody levels increase the risk of differentiated thyroid carcinoma. Disease markers. 2015;2015. http://dx.doi.org/10.1155/2015/648670.
- Anbar M, Guttmann S, Lewitus Z. The mode of action of perchlorate ions on the iodine uptake of the thyroid gland. The International journal of applied radiation and isotopes. 1959;7(2):87-96.
- Singh N, Verma K, Verma P, Sidhu G, Sachdeva S. A comparative study of fluoride ingestion levels, serum thyroid hormone & TSH level derangements, dental fluorosis status among school children from endemic and non-endemic fluorosis areas. SpringerPlus. 2014;3(1):7.
- Pavelka S, Babický A, Vobecký M, Lener J. High bromide intake affects the accumulation of iodide in the rat thyroid and skin. Biological trace element research. 2001;82(1-3):133-142.
- Deveci M, Deveci G, LiVolsi V, Baloch Z. Fine-needle aspiration of follicular lesions of the thyroid. Diagnosis and follow-Up. CytoJournal. 2006;3:9. doi:10.1186/1742-6413-3-9.
- Graham M, Hart R, Douglas S, et al. Serum microRNA profiling to distinguish papillary thyroid cancer from benign thyroid masses. Journal of Otolaryngology – Head & Neck Surgery. 2015;44(1):33. doi:10.1186/s40463-015-0083-5.
- Parsa N. Environmental Factors Inducing Human Cancers. Iranian Journal of Public Health. 2012;41(11):1-9.
- Hutchins-Wolfbrandt A, Mistry A. Dietary turmeric potentially reduces the risk of cancer. Asian Pac J Cancer Prev. 2011;12(12):3169-73.
- Emami A, Reza Nazem M, Hedayati M. Nutritional Protective and Risk Factors of Thyroid Cancer: Still Controversial. Annals Thyroid Res. 2016;2(1):32-33.
- Hosseinimehr S, Hosseini S. Resveratrol sensitizes selectively thyroid cancer cell to 131-iodine toxicity. Journal of toxicology. 2014.
- Mack W, Preston-Martin S, Bernstein L, Qian D. Lifestyle and other risk factors for thyroid cancer in Los Angeles County females. Annals of epidemiology. 2002;12(6):395-401.
- Choi W, Kim J. Dietary factors and the risk of thyroid cancer: a review. Clinical nutrition research. 2014;3(2):75-88.
- Michikawa T, Inoue M, Shimazu T, Sasazuki S, Iwasaki M, Sawada N, et al. Green tea and coffee consumption and its association with thyroid cancer risk: a population-based cohort study in Japan. Cancer Causes & Control. 2011;22(7):985.
- Riza E, Linos A, Petralias A, de Martinis L, Duntas L, Linos D. The effect of Greek herbal tea consumption on thyroid cancer: a case-control study. European journal of public health. 2015;25(6):1001-1005.
- Fernandez E, Chatenoud L, La Vecchia C, Negri E, Franceschi S. Fish consumption and cancer risk. The American journal of clinical nutrition. 1999;70(1):85-90.
- Cancer Network Staff. Obesity Associated With Increased Thyroid Cancer Risk. http://www.cancernetwork.com/thyroid-cancer/obesity-associated-increased-thyroid-cancer-risk. Published October 1, 2015. Accessed January 22, 2018.
- Liu Y, Su L, Xiao H. Review of Factors Related to the Thyroid Cancer Epidemic. International Journal of Endocrinology. 2017;2017:1-10. https://doi.org/10.1155/2017/5308635.
- Lovett I. Health Scare at Malibu School Sets Off Media War. NY Times. https://www.nytimes.com/2016/04/05/us/an-exclusivity-malibu-could-do-without-pcbs.html. Published April 4, 2016. Accessed January 22, 2018.
- Aschebrook-Kilfoy B, Ward M, Valle C, Friesen M. Occupation and Thyroid Cancer. Occupational and environmental medicine. 2014;71(5):366-380. doi:10.1136/oemed-2013-101929.
- García-Niño W, Pedraza-Chaverrí J. Protective effect of curcumin against heavy metals-induced liver damage. Food Chem Toxicol. 2014;69:182-201.
- Tan C, Zhang L, Cheng X, Lin X, Lu R, Bao J, Yu H. Curcumin inhibits hypoxia-induced migration in K1 papillary thyroid cancer cells. Exp Biol Med (Maywood). 2015;240(7):925–935. doi: 10.1177/1535370214555665.
- Xu X, Qin J, Liu W. Curcumin inhibits the invasion of thyroid cancer cells via down-regulation of PI3K/Akt signaling pathway. Gene. 2014;546(2):226-32. doi: 10.1016/j.gene.2014.06.006.
Note: Originally published in April 2016, this article has been revised and updated for accuracy and thoroughness.



 Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Disclosure: As an Amazon Associate I earn from qualifying purchases. We are a professional review site that receives compensation from the companies whose products we review. We test each product thoroughly and give high marks to only the very best. We are independently owned and the opinions expressed here are our own.
Great article! Thank you Izabella for your books and all the information you provide. How often should we get a thyroid ultrasound? My daughter has a large goiter and I have many nodules. I am using Wobenzym daily and last time the biggest nodule was a little smaller! We both have Hashimoto’s. Thank you!
Marlene – thank you so much for your kind words and support! It’s always best to speak to your functional medicine practitioner to evaluate your specific case, and whether you need more testing. Here is a research article which might help further:
TOP 10 THYROID TESTS FOR DIAGNOSIS
https://bruno-michael-wentz.dev01.rmkr.net/articles/top-6-thyroid-tests/
My husband had ptc cancer . They going to remove his tt this month . I wonder any chance we reverse the cancer without surgery Thanks dr
Parminder – thank you for following this page. My heart goes out to you and your husband. Please, understand that due to liability issues, I am unable to answer specific medical questions, but I highly recommend that you work with a functional medicine clinician. It’s an entire medical specialty dedicated to finding and treating underlying causes and prevention of serious chronic disease rather than disease symptoms. Here are some links which might help:
FUNCTIONAL MEDICINE APPROACH TO THE THYROID
https://bruno-michael-wentz.dev01.rmkr.net/articles/functional-medicine-approach-to-the-thyroid
CLINICIAN DATABASE
https://www.thyroidpharmacistconsulting.com/clinician-database.html
MY RECENT CHALLENGES AND FINDING DR. RIGHT
https://bruno-michael-wentz.dev01.rmkr.net/articles/my-challenges-and-finding-dr-right/
I had my thyroid gland removed in 2007 due to Papillary Thyroid Cancer. I never got a diagnosis of Hashimotos before then. Is there any way to test for Hashimotos now, even without a thyroid? I’d like to know if I was/am headed down the autoimmune disease path.
Erica – thank you for reaching out. Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Even when the thyroid is taken out surgically or treated with radioactive iodine the autoimmunity still persists in most cases. Many people will have their thyroids removed, and will develop new autoimmune disorders such as Lupus, Rheumatoid arthritis, etc. The immune system just finds a different target. We need to rebalance the immune system to prevent this. Sometimes the autoimmunity can be reversed as well! The gut determines your immune system. With the exception of discussing proper thyroid medication dosing, the majority of my website and my book focuses on balancing the immune system. The info I present is based on my own research and journey for overcoming my autoimmune thyroid condition. Here are the links to my books:
Hashimoto’s Root Cause
http://amzn.to/2DoeC80
Hashimoto’s Protocol
http://amzn.to/2B5J1mq
Thank you for this breakdown of all the different types of thyroid cancers. I am waiting for Affirma molecular testing results on a “suspicious” biopsy with Hurthle cells. I’ve had multiple nodules for over a decade, my sister had thyroid cancer (no idea what kind), and two years ago I was diagnosed with Hashimotos (goiter, high TPO and thyroglobulin AB levels, normal TSH, T3, and T4). I am very concerned that it is going to be recommended to me to have a thyroid lobectomy only to find out after the fact that all is normal. Not only is this two week waiting period for results a crazy maker, but I don’t like the statistics on how many unnecessary thyroid surgeries are performed. At least I can try to get more information on what type of cells/cancer they think it is if the Affirma comes back inconclusive. I keep wondering if this is a case of too much meddling, that anyone who has thyroid monitoring done is eventually going to have something weird detected that doctors want to remove.
Christy – thank you so much for sharing our journey. I am so sorry you are going through all of this and have had to wait so long for results. My heart goes out to you.<3 The thyroid can break down until it’s almost gone from Hashimoto’s disease. Most thyroid conditions result from the immune system attacking the thyroid because the immune system is out of balance. Even when the thyroid is taken out surgically, is ‘dead’, or treated with radioactive iodine the autoimmunity still persists in most cases. Many people will have their thyroids removed, and will develop new autoimmune disorders such as Lupus, Rheumatoid arthritis, etc. The immune system just finds a different target.
We need to re-balance the immune system to prevent this (sometimes the autoimmunity can be reversed as well). The gut determines your immune system. With the exception of discussing proper thyroid medication dosing, the majority of my website and my books focus on balancing the immune system. The information is based on my own research in my journey whilst overcoming my own autoimmune thyroid condition. Here are some articles which might help:
HASHIMOTOS AND THYROID CANCER
https://bruno-michael-wentz.dev01.rmkr.net/articles/hashimotos-and-thyroid-cancer/
THE CONVENTIONAL, COMPLEMENTARY AND ALTERNATIVE APPROACH TO HASHIMOTO’S AND THYROID CANCER
https://bruno-michael-wentz.dev01.rmkr.net/articles/the-conventional-complementary-and-alternative-approach-to-hashimotos-and-thyroid-cancer
HORMONE REPLACEMENT THERAPY AND CANCER
https://bruno-michael-wentz.dev01.rmkr.net/articles/hormone-replacement-therapy-and-cancer
Is it necessary to have a thyroid biopsy done every 3 years?
Terry – thank you for reaching out. Here is an article you might find helpful:
THYROID NODULES
https://bruno-michael-wentz.dev01.rmkr.net/articles/hashimotos-and-thyroid-nodules/